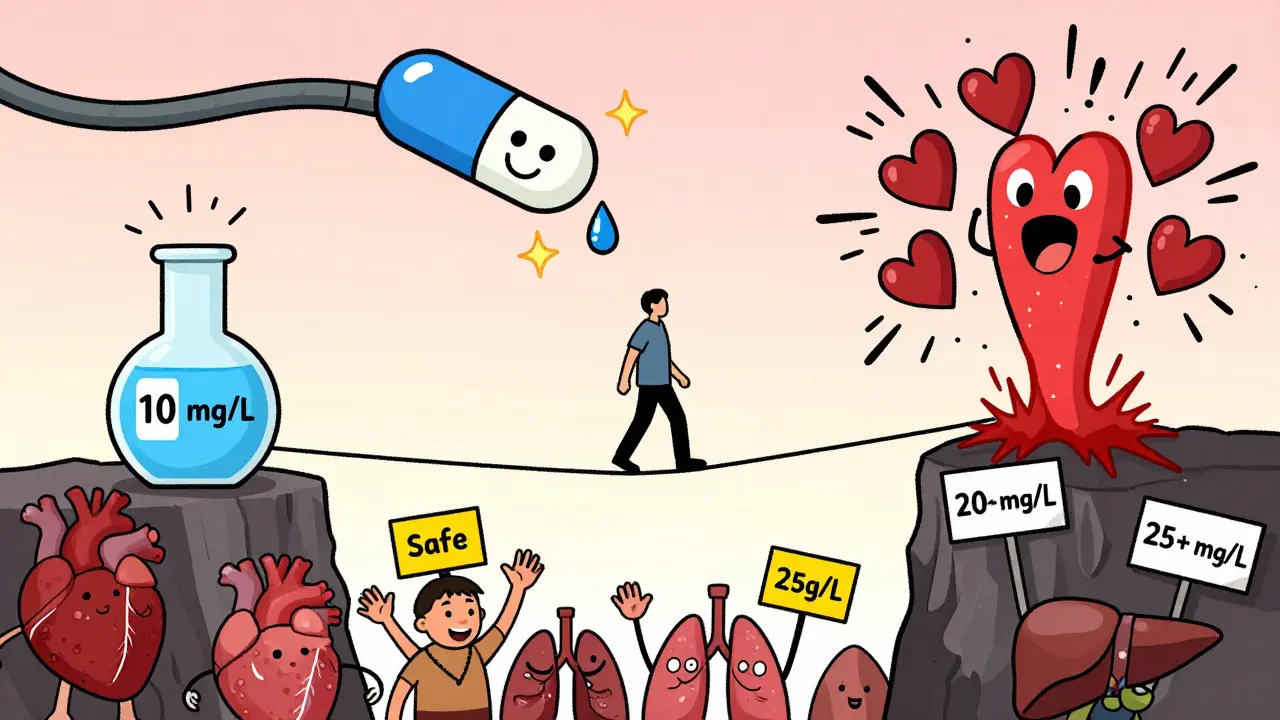
When you take theophylline for asthma or COPD, you’re not just swallowing a pill-you’re walking a tightrope. One milligram too much, and your heart could start racing. One milligram too little, and your lungs might not get the relief they need. That’s because theophylline has a narrow therapeutic index-a tiny window between working and causing harm. And if you’re not monitoring it closely, you’re gambling with your health.
What Makes Theophylline So Dangerous?
Theophylline has been used for over 80 years to open up airways in people with asthma and COPD. It works by relaxing the muscles around the lungs and reducing inflammation. But here’s the catch: the difference between a dose that helps and one that harms is razor-thin. The safe, effective range? Between 10 and 20 mg/L. Go below 10, and it barely works. Rise above 20, and you risk seizures, irregular heartbeats, vomiting, or worse. Above 25 mg/L? That’s a medical emergency.
Why does this happen? Because theophylline doesn’t follow simple rules. Your body doesn’t process it like most drugs. At higher doses, its metabolism slows down and becomes unpredictable. A small increase in your daily dose can cause your blood level to jump by 50% or more. This is called zero-order kinetics-essentially, your liver gets overwhelmed. And that’s just the start.
Your Body Isn’t Like Everyone Else’s
Two people taking the same dose of theophylline can have wildly different blood levels. Why? Because so many factors change how your body handles it.
- Smoking? Your body clears theophylline 50-70% faster. You might need a higher dose-but if you quit, your levels can spike dangerously without warning.
- Drinking alcohol? It can drop your levels, making the drug less effective.
- Age over 60? Liver function slows. Clearance drops. Doses must be lowered.
- Heart failure or liver disease? Clearance can drop by half or more.
- Pregnancy? In the third trimester, your body clears the drug 30-50% faster. Levels can crash, putting both you and your baby at risk.
And then there are the drugs you take alongside it. Antibiotics like erythromycin or clarithromycin can boost theophylline levels by 50-100%. Cimetidine, a common heartburn pill, does the same. Meanwhile, drugs like carbamazepine or St. John’s Wort can slash levels by 30-60%. One new prescription-or a change in your supplements-can turn a stable patient into a patient in crisis.
When and How Often Should You Be Tested?
Monitoring isn’t optional. It’s mandatory. But timing matters.
For immediate-release tablets, blood should be drawn right before your next dose-this is called the trough level. For slow-release forms, samples are taken 4 to 6 hours after taking the pill. Why? Because levels peak and drop differently depending on the formulation.
Here’s the standard schedule:
- Start testing 5 days after beginning treatment-or 3 days after a dose change. That’s how long it takes for levels to stabilize.
- If you’re stable? Check every 6-12 months.
- Over 60? Monitor every 3-6 months.
- Heart failure or liver problems? Every 1-3 months.
- Pregnant? Monthly during the second and third trimesters.
And if you start a new medication, stop smoking, or feel symptoms like tremors, nausea, or a racing heart? Get tested right away. Don’t wait.

What Happens If You Skip Monitoring?
In 2023, a 68-year-old man in Brisbane was admitted to the ER with life-threatening ventricular tachycardia. His theophylline level? 28 mg/L. He’d been on the drug for years. Then his doctor prescribed ciprofloxacin for a sinus infection. Ciprofloxacin blocks the enzyme that breaks down theophylline. Within 72 hours, his levels jumped 65%. He didn’t know. No one tested him. He almost died.
This isn’t rare. Studies show that 15% of theophylline-related hospital visits happen because doctors didn’t adjust doses for liver problems. Another 22% are from unmonitored antibiotic interactions. In one U.S. study, a hospital that started routine theophylline monitoring cut adverse events by 78% and improved asthma control by 35% in just 18 months.
And the problem is getting worse. Between 2020 and 2023, theophylline toxicity cases reported to U.S. poison control centers rose 23% each year. Most victims were elderly, with undiagnosed liver or kidney issues. They weren’t being monitored. They didn’t know the risks.
Beyond Blood Levels: What Else Should Be Checked?
It’s not just about theophylline numbers. You need a full picture.
- Heart rate: Over 100 bpm? That’s a red flag.
- Electrolytes: Low potassium? Common if you’re also on steroids or diuretics. This can make arrhythmias worse.
- Respiratory rate: Is breathing getting harder? Or easier?
- Neurological signs: Headache, insomnia, irritability? These can precede seizures.
- Full blood count: Rare, but theophylline can suppress bone marrow over time.
If you’re getting IV theophylline, the line must be separate from dextrose solutions. Mixing them can cause clumping or even hemolysis. This isn’t a theoretical risk-it’s happened.

Why Do We Still Use Theophylline?
With all these risks, why not just stop using it? Because it still works-especially when other drugs fail.
For people with severe asthma who don’t respond to high-dose inhalers, theophylline adds a powerful anti-inflammatory effect. It helps restore HDAC2, a protein that calms lung inflammation. In low-income countries, it’s one of the few affordable options: a month’s supply costs $15-$30. Compare that to biologic therapies that run $200-$400 a month.
But here’s the truth: it’s not about whether the drug is outdated. It’s about whether you’re managing it right. The European Respiratory Society says it clearly: all theophylline therapy needs monitoring, no matter the dose. Even 200 mg a day isn’t safe without checks.
The Future: Faster Tests, But Still No Shortcuts
Three companies are now testing handheld devices that can measure theophylline levels in under five minutes using a finger-prick sample. If they work, they could change everything-especially for elderly patients who struggle with clinic visits.
But until those devices are approved and widely available, the gold standard remains the same: a lab test. The American College of Chest Physicians says so in their 2024 guidelines. No exceptions. No shortcuts.
There’s no magic here. No quick fix. Just one simple rule: if you’re on theophylline, you need regular blood tests. Not because you’re being difficult. Not because your doctor doesn’t trust you. But because the drug doesn’t care how you feel. It only cares about what’s in your blood.
Ignore the numbers, and you ignore the risk. Monitor them, and you unlock the drug’s real power-without the danger.
How often should theophylline levels be checked?
For most patients, check levels 5 days after starting treatment or 3 days after a dose change. Once stable, monitor every 6-12 months. Higher-risk patients-those over 60, with heart or liver disease, or pregnant-need checks every 1-6 months. Always test after starting or stopping other medications, changing smoking habits, or if symptoms of toxicity appear.
What happens if theophylline levels go too high?
Levels above 20 mg/L increase the risk of side effects. Between 20-25 mg/L, you may experience nausea, vomiting, tremors, or a fast heartbeat. Above 25 mg/L, serious risks kick in: seizures, irregular heart rhythms (like ventricular tachycardia), and even cardiac arrest. Levels over 30 mg/L are often fatal without emergency treatment.
Can I skip blood tests if I feel fine?
No. Theophylline toxicity doesn’t always cause obvious symptoms until it’s too late. Many patients feel fine even as their levels climb into the dangerous range. A 2022 study found that 40% of patients with toxic levels reported no symptoms before hospitalization. Blood tests are the only reliable way to know if your dose is safe.
Which medications interact with theophylline?
Many common drugs affect theophylline. Antibiotics like erythromycin, clarithromycin, and ciprofloxacin can raise levels by 50-100%. Heartburn meds like cimetidine and antifungals like fluconazole do the same. On the flip side, seizure drugs like carbamazepine, tuberculosis drugs like rifampicin, and herbal supplements like St. John’s Wort can lower levels by 30-60%. Always tell your doctor what you’re taking.
Is theophylline still used today?
Yes, but only in specific cases. It’s typically used as a third-line treatment for severe asthma or COPD when inhalers aren’t enough. It’s also common in low-resource settings because it’s cheap. Around 1.2 million people in the U.S. and 850,000 in Europe still use it. But it’s never used without monitoring-its risks demand it.

 Health and Wellness
Health and Wellness
Shalini Gautam
February 21, 2026 AT 12:55Theophylline is one of those old-school drugs that still packs a punch if you know how to handle it. I’ve seen patients in India go from gasping for air to breathing easy on this stuff-no fancy inhalers, no $400 biologics. Just a cheap pill and a blood test. Simple? Yes. Safe? Only if you’re paying attention.
Smokers? They need more. Elderly? Less. Add antibiotics? Watch out. It’s not rocket science-it’s basic pharmacology. But somehow, doctors forget. Maybe because it’s old, maybe because it’s cheap. But that doesn’t make it any less dangerous.
And yet, we still use it. Because when everything else fails, theophylline doesn’t quit. It’s the last soldier standing in the war for breath.
Erin Pinheiro
February 21, 2026 AT 21:31ok so i just read this whole thing and like?? i think we need to ban theophylline?? like i get it its cheap but like what if your liver is just kinda tired?? and your doc forgets to check?? and then you start having seizures?? like why is this still a thing??
also i think the fact that smoking changes everything is wild?? like if you quit smoking you might die?? that’s not a feature, that’s a bug!!
also why is no one talking about the fact that st john’s wort is basically a silent killer here??