Understanding the Emotional Effects of Pulmonary Embolism
Pulmonary embolism (PE) is a serious medical condition that affects not only the physical health but also the emotional wellbeing of the affected individual. It can be a life-threatening condition, and the recovery process can be lengthy and challenging. This section aims to provide an understanding of the psychological impact of pulmonary embolism, focusing on the common emotions experienced by patients, such as anxiety and fear. Recognizing these feelings is the first step towards coping with them and seeking appropriate support.
It is natural for someone who has experienced a pulmonary embolism to feel a range of emotions such as shock, disbelief, anger, sadness, and guilt. However, the most common emotions associated with PE are anxiety and fear. The uncertainty about the future, concerns about recurrent episodes, and the impact on daily life can be overwhelming, leading to increased stress levels and a constant state of worry.
Recognizing Anxiety and Fear after a Pulmonary Embolism
It is important to identify the signs of anxiety and fear after experiencing a pulmonary embolism. These emotions can manifest in various ways, including excessive worry, racing thoughts, irritability, difficulty concentrating, and sleep disturbances. Physical symptoms such as a rapid heartbeat, shortness of breath, chest pain, and dizziness can also be present, which can be particularly concerning for individuals who have experienced a PE, as these are also symptoms of the condition itself.
Being able to recognize these signs is crucial for seeking appropriate help and support. If you find that your anxiety and fear are affecting your daily life, it is important to consult your healthcare provider for guidance. They can help you determine the best course of action to manage these emotions, which may include medication, therapy, or a combination of both.
Seeking Professional Help for Anxiety and Fear
Seeking professional help is an essential step in managing the psychological impact of pulmonary embolism. A mental health professional, such as a psychologist or therapist, can provide valuable support and guidance in coping with anxiety and fear. They can help you develop tools and strategies to manage your emotions, address any underlying issues, and improve your overall emotional wellbeing.
Talking to your healthcare provider about your concerns and feelings can also be beneficial. They can offer reassurance, provide information about your condition and treatment, and recommend appropriate resources and support groups. Remember that it is never too late to seek help, and doing so can significantly improve your quality of life.
Developing Coping Strategies for Anxiety and Fear
Developing effective coping strategies can help you manage your anxiety and fear after experiencing a pulmonary embolism. Some helpful strategies include:
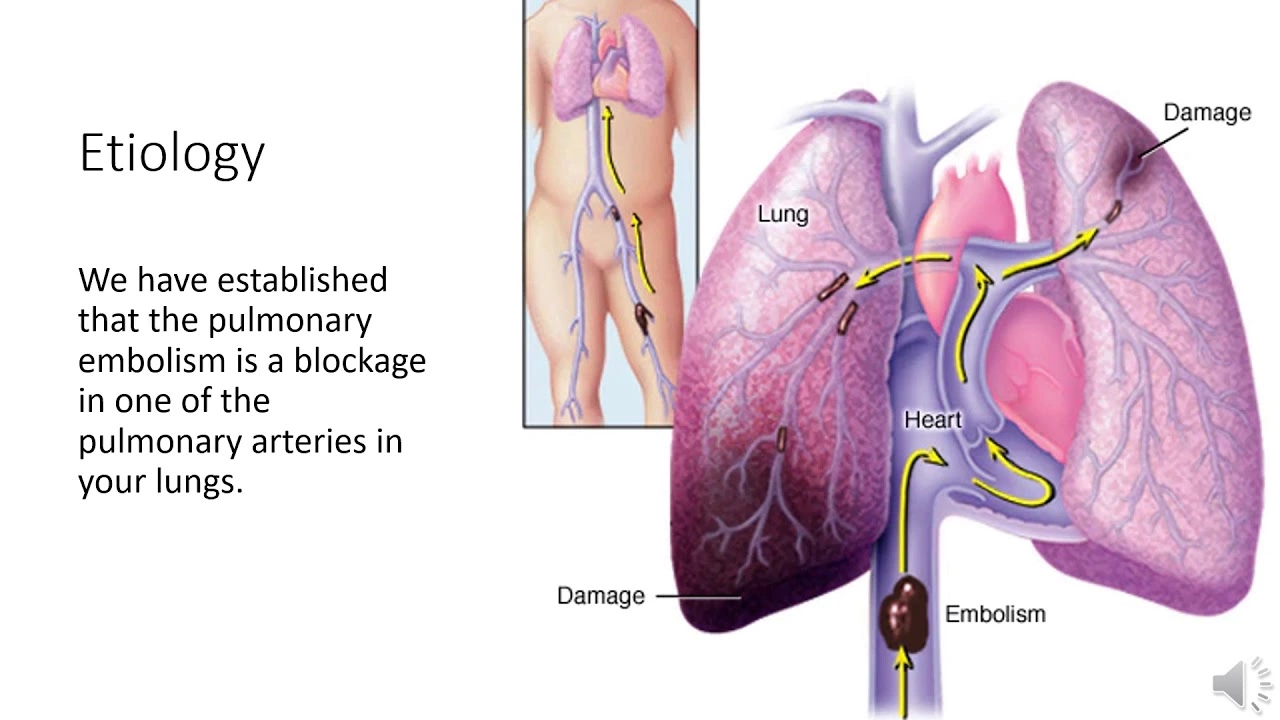
1. Educating yourself about your condition and treatment: Understanding your condition and knowing the facts can help alleviate fear and anxiety. Educate yourself about pulmonary embolism, its causes, symptoms, treatment, and prevention. This can give you a sense of control and empower you to make informed decisions about your health.
2. Practicing relaxation techniques: Techniques such as deep breathing, progressive muscle relaxation, and meditation can help reduce anxiety and promote a sense of calm. Incorporating these practices into your daily routine can help you manage stress and improve your emotional wellbeing.
3. Staying active: Engaging in regular physical activity can help improve mood, reduce stress, and boost overall mental health. Discuss with your healthcare provider the type and intensity of exercise that is appropriate for your specific situation.
Building a Support Network
Having a strong support network is crucial for coping with the psychological impact of pulmonary embolism. Surround yourself with people who understand your situation and can offer encouragement, comfort, and practical assistance. This can include family members, friends, coworkers, or fellow patients who have experienced a similar situation.
Joining a support group specifically for individuals who have experienced pulmonary embolism can also be beneficial. These groups provide a safe space to share your experiences, learn from others, and gain valuable insight into coping strategies and resources. Ask your healthcare provider or search online for a local or online support group.
Focusing on Self-Care
Self-care is an important aspect of managing anxiety and fear after a pulmonary embolism. Taking care of your physical, emotional, and mental health is crucial for your overall wellbeing and recovery. Some self-care strategies include:
1. Eating a balanced diet: A healthy diet can help improve your mood, boost your energy levels, and promote overall health. Focus on incorporating a variety of fruits, vegetables, lean proteins, and whole grains into your meals.
2. Prioritizing sleep: Sleep plays a critical role in emotional wellbeing. Establish a consistent sleep schedule, create a relaxing bedtime routine, and ensure your sleep environment is comfortable and conducive to rest.
3. Engaging in enjoyable activities: Participating in activities that bring you joy and relaxation can help alleviate anxiety and fear. This can include hobbies, spending time with loved ones, or pursuing new interests.
Maintaining Hope and Resilience
Lastly, it is essential to maintain a sense of hope and resilience throughout your recovery process. While it is normal to experience anxiety and fear after a pulmonary embolism, focusing on the progress you have made and the support you have can help you stay positive and motivated. Remember that you are not alone in this journey, and with the right tools and support, you can successfully manage the psychological impact of pulmonary embolism and emerge stronger and more resilient.

 Health and Wellness
Health and Wellness
Michael Barrett
June 18, 2023 AT 15:11In the grand tapestry of human experience, a pulmonary embolism is not merely a physiological event; it is a crucible for the psyche, a test of resilience, and a catalyst for profound introspection. The moment a clot occludes the pulmonary artery, the body sends alarming signals-tachycardia, dyspnea, chest discomfort-that cascade into the mind, igniting a cascade of anxiety that can be as suffocating as the clot itself. One must recognize that fear is not a defect but an adaptive alarm system, a primordial echo of survival that modern medicine has not silenced. Yet, when that echo reverberates incessantly, it morphs into chronic worry, a mental fog that blurs the line between legitimate caution and pathological dread. To disentangle these threads, the patient should first cultivate an accurate mental model of the disease, grounding themselves in epidemiological data that shows recurrence rates are statistically low when anticoagulation is adhered to. This knowledge, when internalized, functions as a cognitive antidote to catastrophizing thoughts. Moreover, the practice of metacognitive awareness-observing one’s own thought patterns without judgment-creates a meta‑layer of control, allowing the individual to intercept spiraling rumination before it hijacks emotional equilibrium.
Neurophysiologically, the amygdala’s hyperactivation in response to perceived threat is amplified by the somatic sensations reminiscent of the original embolic event; thus, body‑mind integration techniques such as diaphragmatic breathing, progressive muscle relaxation, and mindfulness meditation are not mere fluff but empirically supported modalities that attenuate limbic overdrive. In conjunction with pharmacotherapy-selective serotonin reuptake inhibitors when indicated-these practices form a multimodal strategy that addresses both the somatic and the psychic dimensions of recovery. It is also imperative to consider the social scaffold: supportive relationships, peer groups, and patient advocacy networks furnish emotional ballast, buffering against isolation.
Finally, the philosophical perspective reminds us that suffering, while inevitable, can be transmuted into meaning; the narrative of survivorship can become a testament to human fortitude, a story to be shared, a beacon for others navigating the same storm. In sum, the psychological impact of a pulmonary embolism is a complex interplay of neurobiological, cognitive, and social factors, each demanding deliberate attention; only through an integrated approach can one hope to restore equilibrium and emerge, perhaps not unchanged, but undeniably stronger.
Inma Sims
June 24, 2023 AT 21:51Thank you for the exhaustive overview; it is truly enlightening to discover that breathing exercises are the secret weapon against a life‑threatening clot. One can almost feel the surge of optimism as we juggle anticoagulants and mindfulness, as if they were interchangeable. Surely, the mere act of reading this guide will eradicate all lingering fear-no need for professional counseling, right? Your emphasis on “empowerment through knowledge” is remarkably reassuring, especially when the medical jargon is so delightfully accessible. In any case, I commend the effort to transform a serious medical condition into a self‑help checklist; the tone is, as always, impeccably supportive.
Gavin Potenza
July 1, 2023 AT 04:31Honestly, I think the whole anxiety thing is just the mind trying to make sense of something it can’t control; it’s almost philosophical-like confronting the absurd. The article nails that point about grounding yourself in facts, which is key. While I’m all for meditation, I also believe a good walk or a chat with mates does wonders for resetting those racing thoughts. So, blend the science with a bit of ordinary life, and you’ll see the fear recede.
Virat Mishra
July 7, 2023 AT 11:11Another article telling us to breathe and think positive. Yeah right. If only it were that easy. People need real help not just feel‑good fluff. This is just another glossy piece.
Daisy Aguirre
July 13, 2023 AT 17:51Hey there, wonderful warrior! 🌟 Remember, every step you take toward understanding your PE is a victory dance for your spirit. Dive into those breathing exercises, sprinkle in some joyful movement, and let the vibrant community around you lift you higher. You’ve got the power, the passion, and a whole squad cheering you on-keep shining!
Natalie Kelly
July 20, 2023 AT 00:31Hey! Got u covered-talk to ur doc about therapy, try some deep breaths, and stay active. You’ll do great.
Tiffany Clarke
July 26, 2023 AT 07:11I feel your pain deeply
Sandy Gold
August 1, 2023 AT 13:51While the article lauds “relaxation techniques,” let’s not overlook the fact that most studies on mindfulness suffer from methodological flaws-small sample sizes, placebo effects, and the occasional bias. Moreover, the claim that “education alleviates fear” is a stretch; knowledge can sometimes magnify anxiety when patients obsess over statistics. So, before we all start chanting mantras, perhaps a critical appraisal of the evidence is warranted, lest we replace one hype with another.
Frank Pennetti
August 7, 2023 AT 20:31From a clinical perspective, the pathophysiology of PE necessitates a multidisciplinary approach-anticoagulation, hemodynamic monitoring, and psychophysiological interventions must be synergistically integrated. However, the article’s layman language neglects the requisite terminological precision, which could undermine adherence in a nuanced patient cohort. Additionally, the absence of discourse on health policy frameworks limits its applicability within a broader systemic context.
Adam Baxter
August 14, 2023 AT 03:11You got this!
Keri Henderson
August 20, 2023 AT 09:51Remember, you’re not alone in this journey; leaning on friends, family, and support groups can make a huge difference. Keep advocating for yourself, ask questions, and celebrate every small win along the way. Your resilience is inspiring, and we’re all rooting for you.
elvin casimir
August 26, 2023 AT 16:31Let me be clear: adhering to evidence‑based protocols is non‑negotiable, and any deviation constitutes negligence. If you’re still unsure, consult a qualified specialist-self‑diagnosis is a dangerous game, especially in a country that prides itself on medical excellence.
Steve Batancs
September 1, 2023 AT 23:11In the United States, the emphasis on comprehensive post‑PE care reflects our commitment to holistic health, integrating both physical and mental health services. This approach sets a benchmark for other nations seeking to improve patient outcomes.
Ragha Vema
September 8, 2023 AT 05:51It’s almost unbelievable how quickly we’re told to “just breathe” after a potentially fatal clot-who’s really behind that narrative? Some say the pharmaceutical industry wants us dependent on medication, while we’re left to wonder if our fears are truly our own or engineered. Still, sharing our stories can break that invisible chain and bring genuine relief.
Scott Mcquain
September 14, 2023 AT 12:31It is imperative, for the sake of moral integrity, that patients recognize the ethical responsibility to engage in structured psychotherapy; neglecting such duty, while claiming autonomy, reflects a profound misunderstanding of personal accountability; therefore, one must prioritize professional guidance without exception.
kuldeep singh sandhu
September 20, 2023 AT 19:11People love to say “knowledge is power,” yet sometimes too much info just adds noise to the healing process-maybe less is more?
Mariah Dietzler
September 27, 2023 AT 01:51Honestly, the article feels a bit like a checklist without deeper insight; it could use more personal anecdotes to really hit home.
Nicola Strand
October 3, 2023 AT 08:31While the recommendation to join support groups is well‑intentioned, one must consider that not all groups maintain professional oversight, which could lead to the propagation of misinformation; thus, a discerning approach is essential.
Jackie Zheng
October 9, 2023 AT 15:11Let us contemplate the relationship between physiological disruption and psychological turbulence: when the lungs are compromised, the mind perceives a breach in the body’s equilibrium, prompting a cascade of anxiety. Accurate diagnosis and transparent communication serve as anchors, stabilizing the patient’s mental state. Additionally, structured coping mechanisms-such as paced breathing, cognitive reframing, and scheduled physical activity-function as corrective feedback loops, gradually restoring homeostasis. In practice, this synergy between medical treatment and mental‑health support exemplifies the holistic paradigm essential for recovery. Ultimately, fostering resilience is not merely a therapeutic objective but a philosophical pursuit of meaning amidst vulnerability.