
Switching antidepressants isn’t rare-it’s common. About 30% of people on antidepressants will need to change medications at some point. Maybe the first one didn’t help enough. Maybe it caused weight gain, sexual problems, or constant dizziness. Whatever the reason, jumping from one pill to another can be risky if done wrong. The good news? With the right plan, you can make the switch with far fewer side effects and less risk of relapse or worse, serotonin syndrome.
Why People Switch Antidepressants
Most people don’t switch because they want to. They switch because they have to. Around half of those taking SSRIs or SNRIs report side effects that make daily life harder. Sexual dysfunction hits 38-73% of users. Weight gain affects up to 50%. Insomnia, nausea, and brain zaps-those sudden electric-shock feelings in the head-are also common. When these side effects outweigh the benefits, changing meds becomes necessary. But here’s the catch: stopping one antidepressant cold turkey doesn’t just make you feel off-it can trigger withdrawal. Symptoms like dizziness, nausea, headaches, and fatigue can show up within 1-7 days after reducing your dose. For drugs with short half-lives like paroxetine or venlafaxine, these symptoms can hit within 24 hours. That’s why a rushed switch can backfire badly.The Four Ways to Switch
There are four main methods doctors use to switch antidepressants. Not all are equal. Some are safer than others.- Direct switch: Stop the old drug one day, start the new one the next. This is fast, but risky-especially with short-acting meds. It’s rarely recommended unless switching between similar drugs and under close supervision.
- Taper and switch: Slowly reduce the old medication over 1-2 weeks, then stop completely before starting the new one. This reduces withdrawal but leaves a gap where depression can creep back.
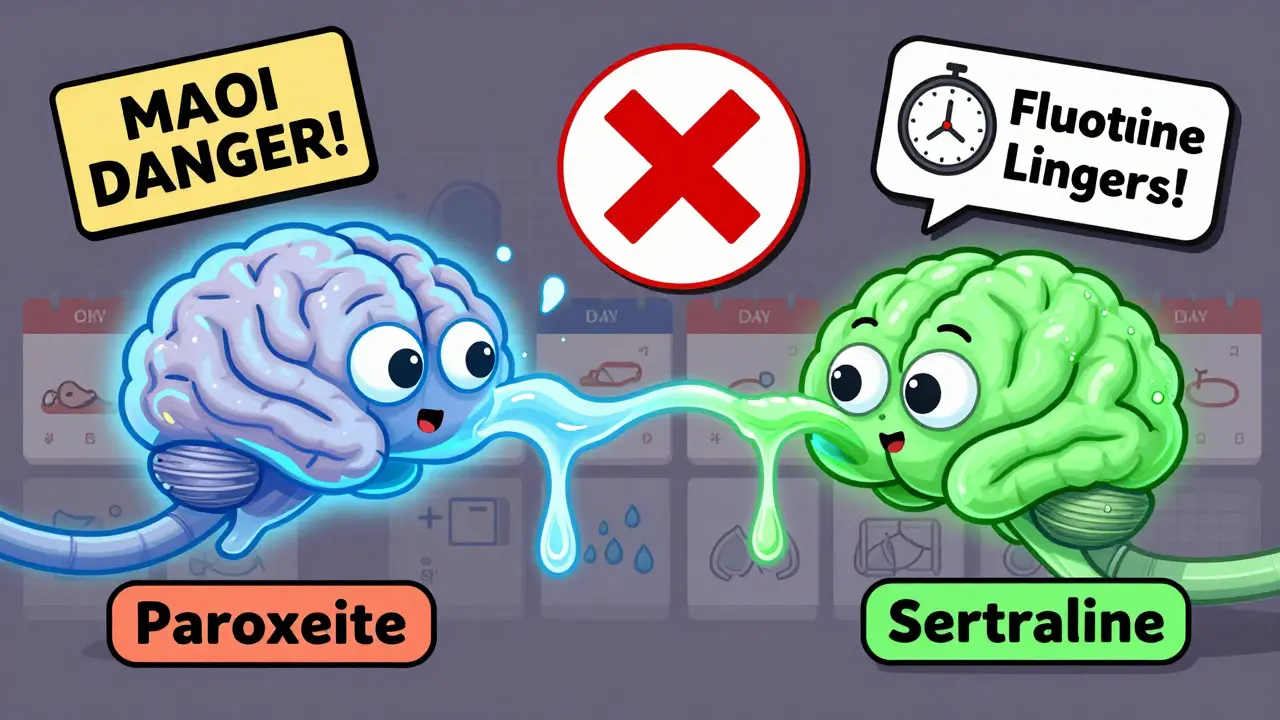
- Taper and switch with washout: Stop the old drug, wait a few weeks, then start the new one. This is required when switching from an MAOI to any other antidepressant, or from fluoxetine to something like clomipramine. Fluoxetine sticks around in your body for up to five weeks after your last dose.
- Cross-taper: This is the gold standard. You slowly reduce the old medication while slowly increasing the new one at the same time. Over 10-14 days, the old one fades out and the new one fades in. This cuts withdrawal symptoms by 42% compared to direct switches, according to a 2021 study.
For most people, cross-tapering is the best choice. It keeps your brain chemistry from crashing. It also gives the new drug time to start working before the old one fully leaves your system.
When a Washout Is Non-Negotiable
Not every switch can be done with a cross-taper. Some combinations are dangerous if mixed-even briefly.- Switching from an MAOI (like phenelzine or tranylcypromine) to any other antidepressant? You need at least a 2-week washout. For fluoxetine, it’s 5 weeks. Why? MAOIs can cause deadly spikes in blood pressure when combined with SSRIs or SNRIs.
- Switching from fluoxetine to a tricyclic (like amitriptyline)? Fluoxetine blocks the liver enzymes that clear tricyclics. That means the tricyclic can build up to toxic levels in your blood. Start low. Go slow. Monitor closely.
- Vortioxetine and duloxetine? These are tricky too. They affect multiple serotonin receptors. Mixing them with other serotonergic drugs increases the risk of serotonin syndrome.
Fluoxetine is the outlier. Because it and its metabolite norfluoxetine linger so long, you can’t just stop and start another drug right away. Rushing this can lead to serious complications. Always check half-lives before switching.
Recognizing Withdrawal vs. Relapse
One of the biggest fears during a switch is: “Is this withdrawal-or is my depression coming back?”- Withdrawal symptoms come on fast-within days. They include dizziness, nausea, brain zaps, electric-shock sensations, insomnia, and flu-like symptoms. They usually improve if you take a small dose of the old medication again. They don’t include low mood, hopelessness, or loss of interest-that’s relapse.
- Relapse symptoms develop slowly over weeks. You feel worse emotionally. You lose motivation. You stop enjoying things. You might have thoughts of hopelessness. These don’t get better with a quick dose of your old pill.
Knowing the difference matters. If you mistake withdrawal for relapse, you might think the new drug isn’t working and quit too soon. If you mistake relapse for withdrawal, you might keep pushing through worsening depression. Always track your symptoms daily during the switch.
Managing Side Effects During the Switch
Even with the best plan, side effects happen. Here’s how to handle them:- Take meds with food. This reduces nausea by about 35%, according to the Mayo Clinic.
- Eat smaller, more frequent meals. Helps your stomach adjust.
- Suck on sugar-free hard candy. Good for dry mouth and nausea.
- Drink plenty of water. Dehydration makes dizziness and fatigue worse.
- Don’t skip sleep. Sleep disturbances are common. Stick to a routine. Avoid caffeine after noon.
- Use liquid formulations if possible. For people who are extra sensitive, liquid antidepressants allow for tiny, precise dose reductions. Some pharmacies can compound them.
Some people report success using low-dose hydroxyzine (an antihistamine) for short-term anxiety or sleep issues during the transition. But never self-prescribe. Talk to your doctor first.
Who Needs Extra Care
Not everyone switches the same way. Some people need more caution:- People under 25: Higher risk of increased suicidal thoughts when starting or switching antidepressants. Check-ins should happen at 1 week after starting the new med, then again at 4 weeks.
- Those on high doses: If you’ve been on more than 40mg of an SSRI daily for over 8 weeks, taper slower. Go over 4-6 weeks, not 2.
- People with heart conditions: Some antidepressants affect heart rhythm. Your doctor may need to do an ECG before and after the switch.
- Those with a history of severe withdrawal: If you’ve had bad reactions before, slow down even more. Some patients need tapers lasting 3-6 months.
There’s no one-size-fits-all. Your doctor should tailor the plan to your history, your body, and your goals.
The Role of Patient Education
A 2022 UK study found something surprising: just explaining what withdrawal symptoms might look like reduced unnecessary medication stops by 37%. When patients know brain zaps aren’t a stroke, or that nausea isn’t a sign the new drug is failing, they stick with the plan.Ask your doctor for a written handout. Write down what symptoms to watch for. Keep a daily journal. Note your mood, sleep, nausea, and any odd sensations. Bring it to your follow-up.
What’s New in Switching
There’s growing interest in two new tools:- Pharmacogenetic testing (like GeneSight): This blood test looks at your genes to predict how you’ll metabolize certain drugs. In a 2022 trial, it improved remission rates by 28%. But it costs around $400 out-of-pocket in the U.S. and isn’t covered by most insurance yet.
- Low-dose naltrexone: Early trials are testing whether this opioid blocker, used in tiny doses, can reduce withdrawal symptoms. In phase 2 studies, it cut discontinuation symptoms by 33%. It’s not standard yet, but it’s promising.
These aren’t magic bullets. But they show the field is moving toward more personalized, safer switches.
What You Should Do Next
If you’re thinking about switching:- Don’t make the decision alone. Talk to your prescriber. Ask: “What’s my goal? What’s the risk if I don’t switch?”
- Ask which switching method they recommend and why. Request a written plan.
- Find out if your current drug has a long half-life. If it’s fluoxetine, paroxetine, or venlafaxine, expect a slower process.
- Ask if you need a washout period. Don’t assume you don’t.
- Get a symptom tracker. Use a simple app or notebook.
- Schedule your first follow-up before you even start the switch. Don’t wait until you feel awful.
Switching antidepressants isn’t a failure. It’s part of finding what works for you. Done right, it can mean relief-not more suffering.
Can I stop my antidepressant cold turkey when switching?
No, except in rare cases. Stopping abruptly increases the risk of severe withdrawal symptoms like dizziness, nausea, brain zaps, and even seizures. Even with fluoxetine-which has a long half-life-it’s safer to taper. Most guidelines strongly recommend gradual reduction over at least 2-4 weeks.
How long do antidepressant withdrawal symptoms last?
For most people, withdrawal symptoms last 1-3 weeks. But if you were on a high dose for a long time, or switched from a short-half-life drug like paroxetine, symptoms can linger for up to 6 weeks. In rare cases, especially with sensitive individuals, they may last longer. If symptoms don’t improve after 4 weeks or get worse, contact your doctor.
Can switching antidepressants cause serotonin syndrome?
Yes, especially if two serotonergic drugs overlap too much. Symptoms include agitation, rapid heart rate, high blood pressure, sweating, shivering, muscle twitching, and confusion. In severe cases, it can lead to fever, seizures, or organ failure. This is why washout periods are required when switching from MAOIs or after fluoxetine. Always tell your doctor every medication you’re taking.
Why is fluoxetine different from other antidepressants?
Fluoxetine has a very long half-life-up to 4-6 days for the drug itself, and its active metabolite, norfluoxetine, lasts 7-15 days. This means it stays in your system for weeks after your last dose. That’s why you need a 5-week washout before starting MAOIs or some tricyclics. It also means withdrawal symptoms from fluoxetine can be delayed and last longer than with other antidepressants.
Is cross-tapering always the best option?
Cross-tapering is the safest and most effective method for most switches, especially between similar drugs like SSRIs or SNRIs. But it’s not always possible. If you’re switching from an MAOI, from fluoxetine to a tricyclic, or if you’re at high risk for serotonin syndrome, a washout is required. Your doctor will choose the method based on your specific meds and health history.
What should I do if I feel worse after switching?
If you feel worse emotionally-more depressed, hopeless, or have thoughts of self-harm-contact your doctor immediately. If you have physical symptoms like high fever, rapid heartbeat, or muscle stiffness, go to the ER. These could be signs of serotonin syndrome. Don’t wait. If symptoms are mild (nausea, dizziness), keep tracking them. Many side effects improve within a week or two. But don’t assume it’s just withdrawal without checking in with your provider.

 Health and Wellness
Health and Wellness
Allen Davidson
January 17, 2026 AT 10:22Just went through this last year switching from sertraline to escitalopram. Cross-taper was a lifesaver. No brain zaps, no nausea, just a quiet shift. Took 12 days, felt like my brain finally stopped screaming. Seriously, don't skip the taper. Your future self will thank you.
Also, liquid formulations? Total game changer. My pharmacy compounding service made me 5mg drops. I could tweak by half a drop. No more guessing games.
john Mccoskey
January 19, 2026 AT 10:01Let’s be real - most people switching antidepressants are just chasing a fantasy. They think the next pill will magically fix their life when the real issue is they refuse to do the work. Therapy. Sleep hygiene. Exercise. Sunlight. These aren’t optional extras - they’re the foundation. Pills are just scaffolding. Stop treating medication like a magic wand and start treating your mental health like something that requires daily discipline.
And yes, serotonin syndrome is terrifying, but it’s also preventable. If you’re too lazy to read the half-life chart or ask your doctor about washouts, you deserve the consequences. This isn’t a video game where you respawn after a bad decision.
Ryan Hutchison
January 19, 2026 AT 16:34U.S. doctors are too scared to taper properly. In Germany, they do cross-tapers in 7 days. Here? You get a 6-week plan and told to ‘be patient.’ Bullshit. The system is broken. Insurance won’t cover compounding pharmacies, so people get stuck with 25mg pills and try to cut them with scissors. That’s not medicine, that’s guesswork.
And don’t even get me started on GeneSight. It’s a $400 placebo wrapped in a lab coat. My cousin got tested, paid out of pocket, got told to switch to fluoxetine - which he’d been on for 8 years. Total waste of money.
Melodie Lesesne
January 20, 2026 AT 22:09Thank you for this. I’ve been on 3 different SSRIs and each switch felt like walking through glass. The brain zaps were the worst - like someone was flicking my skull with a rubber band. I kept thinking I was having mini-strokes. Turns out? Just withdrawal.
Writing down symptoms helped so much. I started a simple notes app: ‘Mood: 4/10, Nausea: yes, Zaps: 3x today.’ Seeing it on paper made me feel less crazy. Also, sugar-free hard candy. I don’t know why it works, but it does.
Corey Sawchuk
January 22, 2026 AT 00:10Fluoxetine is the silent killer of transitions. I didn’t know it stuck around for weeks. Stopped it, started venlafaxine two days later. Ended up in the ER with serotonin syndrome. Not fun. Never again.
Washout periods aren’t suggestions. They’re survival rules. If your doctor doesn’t mention it, ask. Loudly.
Rob Deneke
January 22, 2026 AT 14:31My doc did a direct switch from citalopram to bupropion. I was fine. No issues. Maybe I’m just lucky. But I didn’t taper. Didn’t need to. Some people are just built different.
Also, if you’re on high doses, go slow. I was on 60mg of citalopram for 2 years. Took me 8 weeks to come off. Felt like I was shedding a skin. But worth it.
evelyn wellding
January 23, 2026 AT 08:32THIS. I just switched last month and I’m so glad I found this. I’ve been using the symptom tracker app you mentioned - it’s called Moodfit. Best thing ever. Also, low-dose hydroxyzine helped my anxiety during the taper. My doctor prescribed 10mg at night. No drowsiness, just calm. 🙏
Don’t panic if you feel weird. It’s probably not your brain dying. It’s just adjusting. You got this 💪
Chelsea Harton
January 24, 2026 AT 11:43cross taper works but its not magic. fluoxetine is a beast. dont forget that. and if you think gene sight is worth it you’re delusional. also brain zaps are real. i had them for 6 weeks. not a myth. just sayin.
Corey Chrisinger
January 25, 2026 AT 16:49There’s something deeply human about how we treat our brains like machines we can swap parts on. We don’t think about the soul when we switch meds. We just want the symptoms gone. But what if the symptoms aren’t the enemy? What if they’re the voice of a system trying to tell us something?
Maybe the real question isn’t ‘which pill works best’ - but ‘what are we running from when we keep chasing the next one?’
Just a thought. I’ve been on 7 different antidepressants. I’m not cured. But I’m learning to listen.
Bianca Leonhardt
January 26, 2026 AT 11:11People who say ‘just taper slowly’ clearly haven’t had to do this while working 60-hour weeks and raising kids. You think I have time to track brain zaps and sugar-free candy? I’m not some wellness influencer. I’m just trying to survive.
And if your doctor doesn’t give you a clear plan, find a new one. This isn’t rocket science. It’s basic medical responsibility.
Travis Craw
January 26, 2026 AT 13:49i switched from prozac to zoloft and thought i was gonna die. brain zaps every time i moved my head. i thought it was a tumor. turned out it was just withdrawal. took 3 weeks to settle. i wish i knew then what i know now.
also liquid meds are a blessing. my pharmacy made me 1mg drops. i could go down by 0.5mg at a time. no more cutting pills with scissors
Christina Bilotti
January 27, 2026 AT 01:27Oh look, another article telling people how to ‘safely’ switch antidepressants. How noble. How compassionate. How completely detached from the reality of being a person who’s been on these drugs for a decade and now has to navigate insurance denials, doctors who don’t read the literature, and pharmacies that don’t compound.
Meanwhile, the real issue? We’ve turned depression into a pharmaceutical product line. And you’re just giving people a better instruction manual for the same broken system. Bravo.
brooke wright
January 27, 2026 AT 16:39Wait so if you’re on fluoxetine and want to switch to anything else you have to wait 5 weeks? That’s insane. My doc told me 2 weeks. I did it in 3. I’m fine. Maybe I’m just lucky? Or maybe he was wrong? Should I have gone to the ER? I’m so confused now.
Also, does anyone else get this weird metallic taste when they taper? It’s like licking a battery. It’s not in the article but it happened to me.
vivek kumar
January 29, 2026 AT 01:06As someone from India who switched from sertraline to vortioxetine, I can confirm: cross-taper is the only way. Took 14 days. No withdrawal. No serotonin issues. But I had to pay out of pocket for the liquid formulation - $120. Worth it.
Also, GeneSight isn’t magic but it’s better than nothing. My test showed I’m a slow metabolizer. That’s why I kept getting side effects on standard doses. My doctor adjusted. Game changer.
And yes - fluoxetine’s half-life is a beast. Don’t underestimate it. I saw a guy get serotonin syndrome because he switched too fast. He was 22. Now he’s in rehab. Don’t be that guy.