When you start a new medication, it’s easy to focus on how it’s supposed to help. But the real question isn’t just what it does - it’s what might go wrong. Side effects aren’t rare exceptions. They’re part of the deal. And if you don’t ask the right questions, you could be walking into trouble without even knowing it.
Why am I taking this medicine?
This is the first question you should ask - and it’s not as obvious as it sounds. Many people take medications for years without ever understanding why they were prescribed. A 2023 Cochrane Review found that 15.2% of medications in older adults are continued long after they’re needed. That means someone could be taking a drug for a condition that’s been resolved, or one that’s no longer helping. If your doctor can’t clearly explain the purpose, it’s time to dig deeper. Don’t just accept a prescription. Understand the reason behind it.What are the side effects?
This sounds simple, but most doctors give vague answers like “some people feel dizzy” or “you might have a stomachache.” That’s not enough. You need specifics. Ask: Which side effects are common? Which are serious? And which ones should I never ignore? The Anticholinergic Cognitive Burden Scale (ACB scale), developed in Brisbane, tracks 27 different bodily systems affected by common medications - from dry mouth to confusion. If you’re over 65, or taking more than five medications, you’re at higher risk. A 2019 study found that 6.5% of hospital admissions in adults over 65 were preventable, linked directly to side effects. Don’t settle for a generic list. Ask for the ones that matter to you.What can I do about side effects?
Not all side effects mean stopping the medicine. Some can be managed. For example, if metformin gives you stomach upset, taking it with food cuts that risk by 40%. If you’re on an anticholinergic and get dry mouth, sipping water throughout the day or using sugar-free gum helps. A 2022 University of Sydney study showed 38.7% of patients on these drugs experience dry mouth - and most don’t know simple fixes exist. Ask your doctor: Is there a way to reduce this? Should I change the timing? Can I combine it with something else? Knowing how to handle side effects keeps you on the right treatment - without unnecessary fear.Are there alternatives?
There’s always another option. The Beers Criteria, updated in 2023, lists 56 medications that are potentially inappropriate for older adults because they carry higher risks than benefits. That includes common drugs like diphenhydramine (Benadryl), which can cause confusion and falls. But many doctors don’t bring up alternatives unless you ask. Ask: Is there a safer drug? A non-drug option? A lower-dose version? A 2022 NEJM study showed that combining blood thinners with ibuprofen increases bleeding risk by 2.8 times. If you’re on both, you need to know. Don’t assume your current prescription is the only choice.Do I still need to take this medicine?
Medications aren’t forever. Many people keep taking pills long after they’re needed. A 2023 study found that 15.2% of prescriptions in older adults are continued unnecessarily. Maybe your blood pressure is now controlled. Maybe your pain has improved. Maybe the original reason doesn’t apply anymore. Ask your doctor: Should I keep this? Can I try stopping it? Is there a way to taper off safely? Deprescribing - carefully reducing or stopping medications - is now a recognized part of good care. It’s not giving up. It’s protecting yourself.
What constitutes a serious side effect?
Not every weird feeling means an emergency. But some do. The FDA defines serious side effects as events that cause death, hospitalization, disability, birth defects, or are life-threatening. That’s not vague. It’s specific. Ask your doctor: Which side effects require me to call you right away? Which mean I need to go to the ER? If you feel chest pain, sudden confusion, swelling in your throat, or severe rash - those are red flags. But if you’re unsure, you need a clear line drawn. A 2023 FDA report showed 4.2% of adverse events led to hospitalization. You should know if you’re in that group.Will this medicine interact with anything else I’m taking?
This is where things get dangerous. Most people don’t realize that over-the-counter drugs, supplements, or even grapefruit juice can clash with prescriptions. The Lexicomp database tracks over 1,200 drug interactions. One of the most common? Taking blood thinners with ibuprofen or naproxen. That combination can double your bleeding risk. Or mixing antidepressants with certain herbal supplements - which can trigger serotonin syndrome. Ask: What about my vitamins, painkillers, or sleep aids? What about my neighbor’s cough syrup? Is this safe with my other meds? A 2024 FDA MedWatch review found 63.2% of serious adverse events involved patients who didn’t ask about OTC interactions.Should I take this with or without food?
Food changes how your body absorbs medicine. Some drugs work better with food. Others cause nausea if taken with it. A 2023 FDA report says food affects 40% of medications. If you’re told to take something “on an empty stomach,” what does that mean? Two hours before? After a snack? Ask for clear instructions. If you’re told “take with water,” does that mean any liquid? Can you take it with coffee? These details matter. One wrong habit can make your medicine less effective - or more toxic.Is there a cheaper or generic version?
Cost isn’t just a wallet issue - it’s a safety issue. A 2022 FDA study showed generics save patients 89.1% on average. But if you can’t afford your medicine, you’ll skip doses, cut pills, or stop entirely. That’s when things go wrong. Ask: Is there a generic? Is it as safe? Will my insurance cover it? If the answer is no, ask if there’s another drug that’s cheaper. Many patients don’t ask because they assume cost is fixed. It’s not. Your doctor can often switch you to a lower-cost option that works just as well.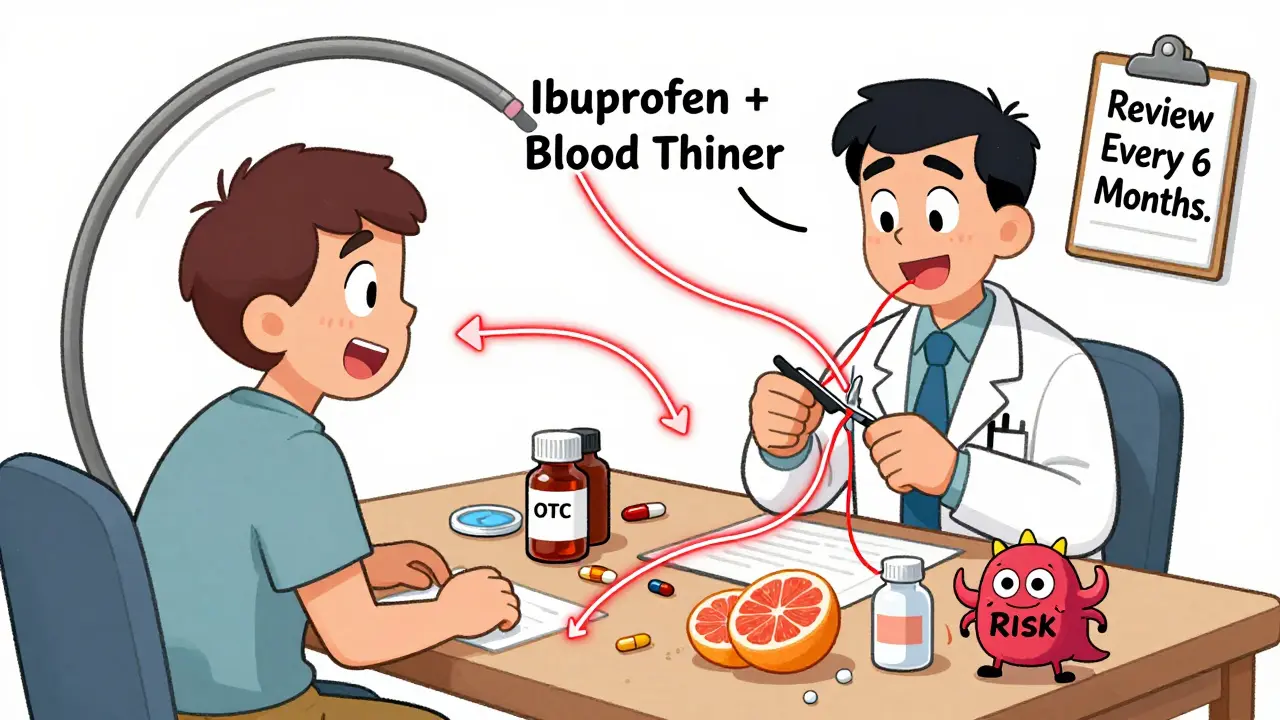

 Health and Wellness
Health and Wellness
Kathryn Lenn
February 8, 2026 AT 03:42John Watts
February 9, 2026 AT 23:56Randy Harkins
February 10, 2026 AT 06:23Chima Ifeanyi
February 11, 2026 AT 03:40Elan Ricarte
February 11, 2026 AT 21:08Angie Datuin
February 12, 2026 AT 14:30Camille Hall
February 14, 2026 AT 01:38Ritteka Goyal
February 14, 2026 AT 08:32