
Why legitimate drug sourcing isn’t optional-it’s life or death
Every pill, injection, or capsule your pharmacy orders has a story. Where did it come from? Who made it? Was it stored correctly? If you can’t answer those questions with certainty, you’re gambling with people’s lives. In 2023, the FDA confirmed that counterfeit drugs still make up about 1% of the global supply. That might sound small, but it’s over $200 billion in fake medicine circulating every year. And it’s not just overseas-fake insulin, cancer drugs, and antibiotics are showing up in U.S. pharmacies too.
Legitimate drug procurement isn’t about paperwork for the sake of compliance. It’s about building a wall between patients and dangerous products. The rules aren’t suggestions. They’re federal law. And if you’re running a pharmacy, you’re on the front line.
The DSCSA: The backbone of U.S. drug traceability
The Drug Supply Chain Security Act (DSCSA), passed in 2013 and fully enforced by November 27, 2023, changed everything. Before this law, a drug could move from manufacturer to wholesaler to pharmacy with no digital trail. Now, every transaction must be recorded electronically. That means:
- Each package has a unique serial number
- Every transfer comes with transaction information, history, and a statement
- All trading partners must exchange data in a standardized, interoperable format
This system lets you trace a drug back to the factory in minutes-if the data is complete. But here’s the catch: 58% of pharmacies still struggle with missing or corrupted transaction data from suppliers. One hospital in Ohio had to quarantine $87,000 worth of medication last year because a distributor’s system glitched during the DSCSA upload. That’s not an anomaly-it’s the new normal for under-resourced pharmacies.
Who can you trust? Supplier vetting checklist
You don’t buy from just anyone. The American Society of Health-System Pharmacists (ASHP) lays out seven non-negotiable criteria for choosing suppliers:
- Current FDA registration and state pharmacy license
- Proof of cGMP (current Good Manufacturing Practices) compliance
- Documented quality management system
- No history of recalls or adverse events in the last 3 years
- Security measures to prevent theft or diversion
- Financial stability (no red flags like sudden bankruptcy filings)
- Full DSCSA compliance-no exceptions
Most independent pharmacies don’t have the staff to do this manually. That’s why 89% of hospitals using group purchasing organizations (GPOs) reported zero supply chain incidents in 2022. Meanwhile, 65% of independent pharmacies spend over 10% of their budget just on compliance. If you’re doing this alone, you’re at a massive disadvantage.
Barcode scanning isn’t optional-it’s your last line of defense
Even with perfect paperwork, a fake drug can slip through if you don’t physically verify it. ASHP recommends scanning every single incoming pharmaceutical item. Why? Because NDCs (National Drug Codes) and lot numbers on fake labels can look real-until you scan them and the system says, “No match.”
Imagine this: You get a shipment of metformin. The box looks right. The label looks right. But when you scan the barcode, your ERP system flags it as expired and mismatched to your purchase order. That’s not a glitch-that’s your system saving a patient from a dangerous dose. One pharmacy in Michigan stopped a counterfeit batch of warfarin this way. The fake pills had the right NDC, but the lot number didn’t exist in the manufacturer’s database.
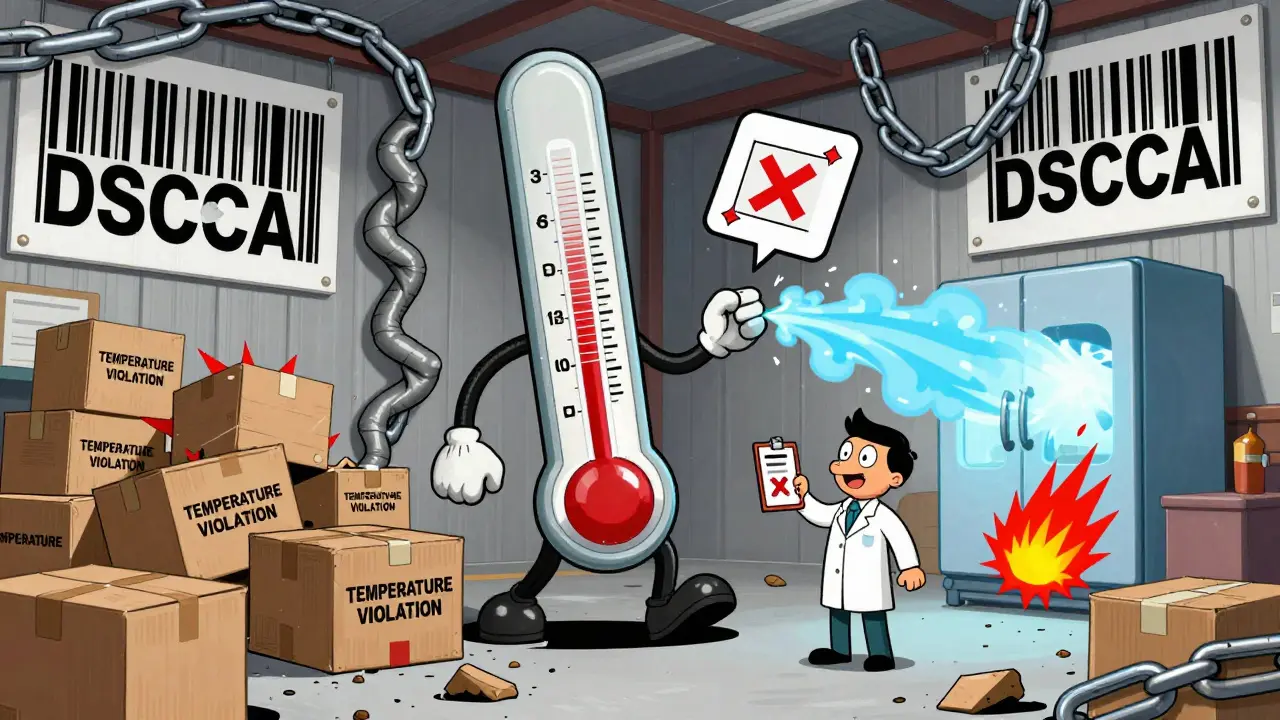
Temperature control: The silent killer
Some drugs aren’t just fake-they’re ruined. Insulin, vaccines, biologics-they all need cold storage. The standard? 2°C to 8°C. Go outside that range for even a few hours, and the drug loses potency. You won’t see a label saying “this is bad.” The patient just won’t get better.
Legitimate suppliers must have temperature monitoring logs for every shipment. You need to check those logs when the package arrives. If the temperature went above 10°C during transit? Quarantine it. Document it. Report it. Don’t assume it’s fine because the box felt cool. One hospital in Texas had 12 patients develop severe infections after receiving degraded antibiotics that weren’t properly refrigerated. The supplier claimed it was “a one-time issue.” It wasn’t.
White bagging vs. brown bagging: The hidden risks
You might think specialty drugs are safe because they’re expensive. But here’s the truth: the more complex the supply chain, the more opportunities for fraud.
- White bagging: A specialty pharmacy ships the drug directly to your facility. Sounds clean? Not always. If the pharmacy isn’t DSCSA-compliant, you’re taking in unverified product.
- Brown bagging: The patient brings the drug from their retail pharmacy. No chain of custody. No traceability. No documentation. This method is still used in 30% of oncology clinics-and it’s the top cause of medication errors in specialty care.
ASHP found that 42% of health systems using nontraditional supply chains had at least one medication error tied to improper handling. That’s not a glitch. That’s systemic failure.
The hidden cost of cutting corners
Buying from a cheaper, unverified supplier might save you $500 on a single order. But here’s what it really costs:
- Regulatory fines: Up to $10,000 per violation under FDA rules
- Product recalls: Average cost of $1.2 million per incident
- Reputation damage: Patients leave when they find out you sold fake drugs
- Lawsuits: One wrongful death case tied to counterfeit antibiotics cost a pharmacy chain $27 million in 2022
And don’t forget the human cost. A 68-year-old woman in Indiana died after taking fake metformin that contained toxic levels of NDMA. The supplier? A distributor with no FDA registration. The pharmacy? They didn’t scan the lot number.

What’s changing in 2025-2026
The rules are tightening. The FDA is getting more funding-$150 million more in 2024 than in 2023. By 2026, 90% of pharmaceutical transactions are expected to use AI to detect anomalies in supply chain data. That means systems will automatically flag:
- Unusual shipping routes
- Discrepancies in batch sizes
- Suppliers with no prior transaction history
Blockchain-based verification platforms like TraceLink and rfxcel are already being adopted by 73% of large hospitals. They’re not perfect-but they’re closing the loopholes counterfeiters rely on.
But here’s the reality: technology won’t fix a culture of laziness. If your staff skips scanning because it’s “too slow,” or if you accept supplier docs without verifying them, no AI in the world will save you.
What you need to do right now
If you’re a pharmacy owner or manager, here’s your action list:
- Confirm every supplier has current FDA registration and state license-don’t take their word for it. Check the FDA’s website yourself.
- Implement 100% barcode scanning for all incoming drugs. Use your ERP system to auto-match NDCs and lot numbers.
- Require temperature logs for every refrigerated shipment. Store them digitally for at least 6 years.
- Train your staff. 120 hours of DSCSA and cGMP training isn’t optional-it’s the bare minimum.
- Join a GPO if you’re independent. The compliance support alone is worth the fee.
- Designate a compliance officer. 92% of hospitals with a Chief Pharmacy Officer have zero major incidents.
There’s no shortcut. No hack. No “we’ve always done it this way.” The system is built to protect you-and your patients. Use it. Or risk becoming the next headline.
What happens if my pharmacy receives a counterfeit drug?
You must immediately quarantine the product, notify the FDA through their MedWatch system, and report it to your supplier. You’re also required to investigate how it entered your supply chain and document your corrective actions. Failure to report can result in fines, loss of license, or criminal charges. The FDA tracks these reports closely-repeat offenders face shutdowns.
Can I buy drugs from international suppliers?
Technically, no-unless they’re FDA-approved and meet DSCSA standards. Most international suppliers, even those based in Canada or the EU, aren’t registered to sell directly to U.S. pharmacies. Drugs imported from outside the U.S. supply chain are considered unapproved and illegal, regardless of whether they’re genuine. The FDA has seized thousands of shipments from overseas sellers posing as legitimate distributors.
Do I need to verify every single lot number?
Yes. Every single one. Even if you’ve bought from the same supplier for 20 years. Counterfeiters often use real NDCs from legitimate products but put them on fake pills. The only way to catch that is by matching the lot number to the manufacturer’s database through your scanning system. Skipping this step is like locking your door but leaving the key under the mat.
How often should I audit my suppliers?
At least quarterly. You need to re-verify licenses, check for new recalls, review their DSCSA compliance records, and confirm their financial stability. Some suppliers get bought out, change ownership, or lose their certifications without telling you. A yearly check isn’t enough-counterfeiters move fast, and so should your verification.
What’s the difference between 503A and 503B compounding pharmacies?
503A pharmacies compound custom prescriptions for individual patients under state oversight. 503B outsourcing facilities produce larger batches for multiple facilities and must follow FDA cGMP standards. If you’re buying compounded drugs from a 503B, you must verify they’re registered with the FDA and listed on the official directory. Many counterfeit drugs are sold as “503B compounded” when they’re not. Always check the FDA’s list before ordering.
Can I use a third-party logistics company to store my drugs?
Only if they’re licensed as a wholesale distributor and registered with the FDA. Third-party logistics providers (3PLs) must be VAWD-accredited or hold equivalent state licenses. You’re still responsible for the drugs in their care. If they fail to maintain temperature controls or lose tracking data, you’re liable. Never outsource compliance-it’s your duty.
Final thought: This isn’t about rules-it’s about responsibility
You didn’t become a pharmacist to chase savings. You became one to help people. Every time you skip a scan, ignore a temperature log, or accept paperwork without verification, you’re not saving time-you’re risking lives. The system is complex, yes. But it’s built to protect you. Use it. Fully. Faithfully. Because in this line of work, there’s no room for shortcuts.

 Health and Wellness
Health and Wellness
Kunal Majumder
January 9, 2026 AT 03:37Ted Conerly
January 9, 2026 AT 13:17Jaqueline santos bau
January 11, 2026 AT 02:56anthony martinez
January 13, 2026 AT 01:44Mario Bros
January 14, 2026 AT 08:40neeraj maor
January 15, 2026 AT 13:23Ashlee Montgomery
January 16, 2026 AT 10:43Paul Bear
January 18, 2026 AT 10:36chandra tan
January 20, 2026 AT 02:45Saumya Roy Chaudhuri
January 20, 2026 AT 21:43McCarthy Halverson
January 22, 2026 AT 03:30Dwayne Dickson
January 23, 2026 AT 02:49Faith Edwards
January 23, 2026 AT 16:12Jake Kelly
January 24, 2026 AT 03:37Ritwik Bose
January 25, 2026 AT 03:09