
When someone is fighting advanced cancer, the goal shifts from curing the disease to making life as comfortable as possible. This is where palliative care comes in-not as a last resort, but as a vital part of treatment from the very start. The truth is, 70 to 90% of people with late-stage cancer experience serious pain. And yet, far too many still suffer needlessly. The good news? Up to 90% of that pain can be controlled with the right approach. It’s not about giving up. It’s about living better, with less suffering.
What Does Palliative Care Actually Do?
Palliative care isn’t hospice. It’s not about stopping treatment. It’s about adding support. A palliative care team works alongside oncologists to tackle pain, nausea, fatigue, anxiety, and emotional distress. Their job? To help patients stay as active and comfortable as possible, even while undergoing chemo, radiation, or surgery. The focus is simple: reduce suffering and improve daily life.Studies show that when palliative care starts early-within eight weeks of diagnosis-patients report 20 to 30% better quality of life. Some even live longer. One major study found that metastatic cancer patients who got early palliative care lived 2.5 months longer on average than those who didn’t. That’s not magic. That’s science.
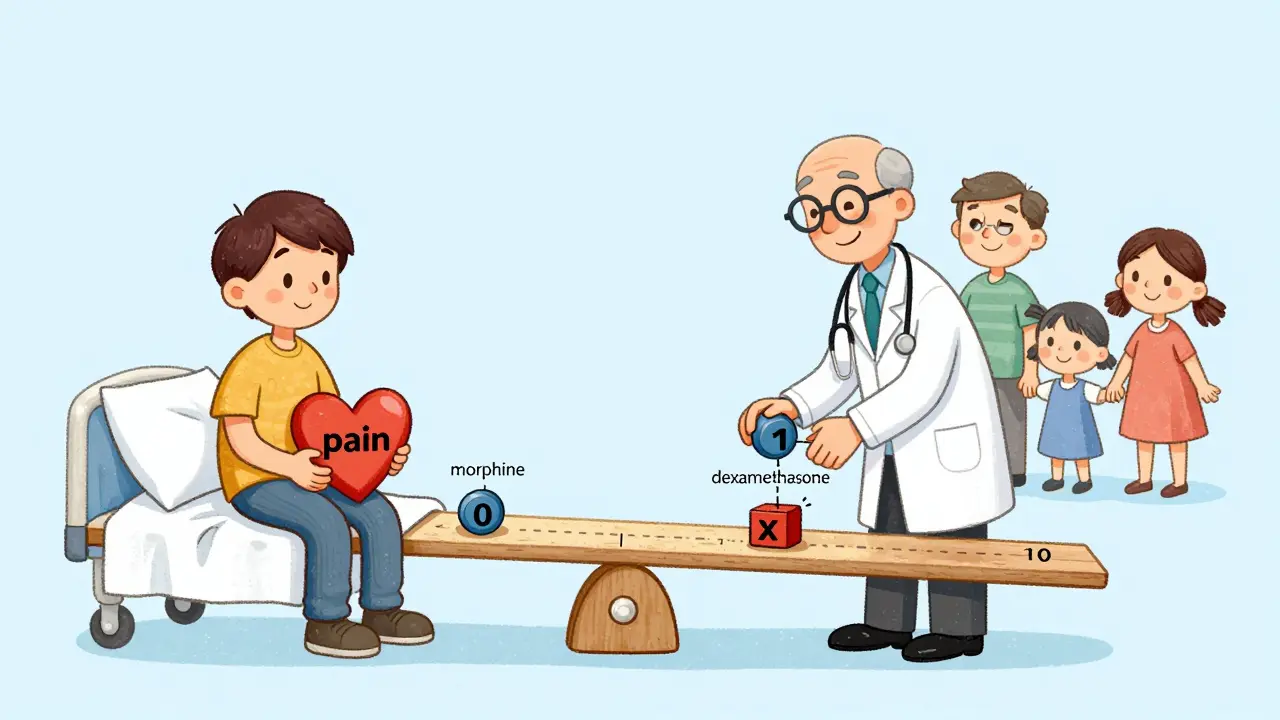
How Is Cancer Pain Measured?
You can’t treat what you can’t measure. That’s why every cancer center now uses a 0-to-10 pain scale. Zero means no pain. Ten means the worst pain you can imagine. Doctors ask this question at every visit: On a scale of 0 to 10, how much pain are you in right now? It sounds simple, but it’s the most reliable tool we have.But pain isn’t just a number. A good assessment looks at:
- Where the pain is (bone? abdomen? nerves?)
- What it feels like (sharp? burning? aching?)
- When it happens (constant? only at night? worse when moving?)
- What makes it better or worse
- How much it interferes with sleeping, eating, or talking
Tools like the Brief Pain Inventory and McGill Pain Questionnaire help capture this full picture. Without this detail, doctors are guessing. With it, they can match the treatment to the pain.
The Three-Step Ladder for Pain Relief
The World Health Organization’s analgesic ladder is still the backbone of cancer pain treatment. It’s straightforward, effective, and used worldwide.Step 1: Mild pain (1-3)
- Acetaminophen: Up to 4,000 mg per day (no more-overdose can damage the liver)
- NSAIDs: Ibuprofen (400-800 mg three times daily) or naproxen. These help with inflammation and bone pain.
Step 2: Moderate pain (4-6)
- Add a weak opioid: Codeine (30-60 mg every 4 hours) or tramadol
- Still use acetaminophen or NSAIDs together
Step 3: Severe pain (7-10)
- Switch to a strong opioid: Morphine (5-15 mg every 4 hours orally) is the most common starting point
- Dosing isn’t fixed-it’s adjusted. If pain isn’t controlled after 24 hours, the dose goes up by 25-50%
- Breakthrough pain? Give 10-15% of the total daily dose as a rescue dose
This isn’t about addiction. It’s about control. People with cancer aren’t using opioids for fun. They’re using them to breathe, sleep, or hug their grandchild without crying.
What If Opioids Don’t Work or Cause Side Effects?
Not everyone responds the same way. Some get dizzy. Others feel nauseated. A few develop a strange sensitivity to pain called opioid-induced hyperalgesia-where the medicine makes the pain worse. That’s when you switch.Doctors use equianalgesic tables to convert one opioid to another. If morphine isn’t working, they might switch to hydromorphone, fentanyl, or methadone. But here’s the catch: when switching, they start at 50-75% of the calculated dose. Why? Because the body doesn’t fully tolerate the new drug right away. Too much can cause breathing problems.
For bone pain from metastases, radiation therapy is often more effective than pills. A single 8-gray radiation session can knock out pain in days. Sometimes, doctors combine it with zoledronic acid (4 mg IV every 3-4 weeks), which strengthens bones and reduces fractures.
Medicines That Help Beyond Opioids
Pain isn’t just about the nerves firing. Sometimes, it’s caused by nerve damage, inflammation, or pressure. That’s where adjuvant drugs come in:- Gabapentin or pregabalin: For nerve pain (neuropathy) from chemo or tumors pressing on nerves. Dose: 100-1,200 mg three times daily
- Duloxetine: An antidepressant that also blocks pain signals. 30-60 mg daily helps with both pain and depression
- Dexamethasone: A steroid that reduces swelling around tumors. 4-16 mg daily can ease bone or brain pain
- Bisphosphonates: Used with radiation for bone metastases
These aren’t optional extras. They’re essential tools. A patient with bone pain might need morphine + dexamethasone + radiation. A patient with burning nerve pain might need gabapentin + duloxetine. It’s not one-size-fits-all.
Why Do So Many People Still Suffer?
Even with all this knowledge, pain is still undertreated. Why?- Doctors don’t ask: A 2017 study found 40% of oncology nurses weren’t certified in pain management. If the team doesn’t check, the pain goes unnoticed.
- Patients don’t speak up: Over 65% of patients fear addiction or think pain is just part of cancer. Some cultures encourage silence-Asian and Hispanic patients underreport pain 28% more often due to stoicism.
- Insurance won’t cover it: Physical therapy, acupuncture, counseling-these help, but many plans don’t pay for them.
And then there’s the fear of opioids. The CDC warns against high doses for chronic non-cancer pain. But cancer pain is different. The goal isn’t to avoid opioids-it’s to use them safely and effectively. The 2022 CDC update even added a special exception for cancer patients.

What Happens If Pain Isn’t Controlled?
Uncontrolled pain doesn’t just hurt. It steals everything:- It stops you from eating
- It keeps you awake
- It makes you anxious or depressed
- It isolates you from family
- It can even shorten your life
When pain is managed well, patients can travel. Visit friends. Laugh. Watch a sunset. That’s not a luxury. That’s dignity.
How to Get Better Pain Care
If you or a loved one has cancer, here’s what to do:- Ask for a pain assessment at every appointment. Don’t wait until it’s unbearable.
- Use the 0-10 scale. Say the number out loud. Write it down.
- Ask: Is this pain being treated the right way?
- Request a palliative care consultation. You don’t need to be near death to get it.
- Ask about non-opioid options: radiation, steroids, nerve blocks, physical therapy.
- Bring a family member to appointments. They can help remember details and speak up if you’re too tired.
And if your doctor says, We can’t give you more pain medicine, ask why. Is it fear? Policy? Lack of training? Push for a second opinion. You have the right to live without unnecessary suffering.
The Future of Cancer Pain Management
New tools are coming fast. Apps now let patients log pain in real time-studies show 22% better documentation accuracy. Genetic tests can tell if your body metabolizes opioids slowly, so doctors can adjust doses before side effects happen.Researchers are testing 12 new drugs targeting cancer-specific pain pathways, like nerve compression and bone destruction. One day, we might have pills that block pain without opioids at all.
But the biggest breakthrough isn’t a drug. It’s the shift in mindset: Palliative care isn’t giving up. It’s fighting for quality. And that fight starts with one simple question: How much pain are you in today?
Is palliative care only for people who are dying?
No. Palliative care is for anyone with a serious illness like cancer, no matter the stage. It can start at diagnosis and continue alongside treatments like chemotherapy or surgery. The goal is to improve daily life-not to stop treatment.
Will opioids make me addicted if I use them for cancer pain?
The risk of addiction is very low when opioids are used properly for cancer pain. Most patients take them for weeks or months, not years. Their body needs them to manage real, physical pain-not for pleasure or escape. Doctors monitor closely and adjust doses to avoid dependence.
What if my pain medicine stops working?
This is common. The body can build tolerance, or the cancer may spread. Doctors don’t just increase the dose-they may switch to a different opioid, add an adjuvant drug like gabapentin, or use radiation to target bone tumors. Pain that doesn’t respond to one method often responds to another.
Can non-drug treatments help with cancer pain?
Yes. Radiation therapy can relieve bone pain in days. Nerve blocks, physical therapy, acupuncture, and massage help many patients. Counseling and mindfulness reduce the emotional weight of pain, which often makes the physical sensation feel less intense.
Why do some patients underreport their pain?
Some fear being seen as weak. Others worry about addiction, or believe pain is just part of having cancer. Cultural norms in some communities encourage silence. Patients may also fear that reporting pain means their cancer is worsening. Doctors need to create safe spaces to talk openly about pain without judgment.

 Health and Wellness
Health and Wellness
Josiah Demara
February 14, 2026 AT 22:31Let me break this down for you people who think palliative care is some kind of soft option. You're not 'making life comfortable'-you're surrendering to the inevitable. The WHO ladder? That's a 1986 relic. Modern oncology uses targeted neuromodulators, spinal cord stimulators, and intrathecal drug delivery systems. You're still talking about morphine and ibuprofen like we're in the Stone Age. And don't get me started on 'adjuvant drugs'-gabapentin for nerve pain? That's just throwing darts at a board while the tumor eats your spine. Real pain control requires precision, not poetry.
Kaye Alcaraz
February 16, 2026 AT 14:49Thank you for this clear, science-backed guide. It’s rare to see such a thorough breakdown of pain management that doesn’t reduce patients to statistics. The emphasis on early intervention and multidisciplinary care is exactly what we need. Every oncology team should be required to have a palliative care specialist embedded from day one. Quality of life isn’t a luxury-it’s the foundation of dignity. This should be mandatory reading for all medical students.
Charlotte Dacre
February 17, 2026 AT 20:09Oh wow. A 70-page pamphlet disguised as a Reddit post. Next you'll tell us to 'use the 0-10 scale' while holding a candle and whispering to our tumors. I love how the article treats pain like a math problem you can solve with a flowchart. 'Add tramadol, wait 4 hours, check if you're still sobbing.' Meanwhile, real people are lying in bed wondering if their grandkids will remember them as a person or just a 'pain case.'
Esha Pathak
February 19, 2026 AT 17:07There is a deeper truth here beyond pills and scales. Pain is not just a physical phenomenon-it is the soul screaming in a world that has forgotten how to listen. When we reduce human suffering to a 0-10 score, we are not treating pain-we are sanitizing it. The body remembers trauma. The spirit remembers abandonment. No opioid can heal the silence between a mother and her child who can no longer hug without crying. We must return to presence, not protocols.
Sarah Barrett
February 19, 2026 AT 20:59This is one of the most comprehensive and clinically accurate summaries of cancer pain management I’ve seen in a public forum. The distinction between palliative care and hospice is consistently misunderstood, and the data on early intervention improving survival is compelling. The inclusion of non-opioid adjuvants and radiation protocols reflects current NCCN guidelines. Kudos to the author for avoiding sensationalism and sticking to evidence.
Mike Hammer
February 20, 2026 AT 13:53man i had my grandma on this stuff last year. doc said 'start with 5mg morphine' and i was like 'wait, that's it?' then she was able to eat pizza again. no joke. that's what this is about. not science jargon. not ladder steps. just being able to laugh without it hurting. also the radiation thing? she got one session and said her hip felt like it had been unglued. like magic. but magic that's backed by science. also bring snacks to appointments. they always forget to tell you about the nausea pills.
Daniel Dover
February 22, 2026 AT 11:09Early palliative care improves survival. That's the key takeaway.
Joe Grushkin
February 23, 2026 AT 09:02Let me guess-this was written by a hospital marketing team trying to sell more 'compassionate care' packages. You mention 'dignity' and 'sunset' like it's a Hallmark movie. Meanwhile, real cancer patients are getting denied insurance for nerve blocks because they're 'experimental.' And you act like opioids are harmless? You think people don't know about the black market for morphine? This isn't empowerment-it's sanitized propaganda for people who still believe in the myth of the benevolent medical system.
Virginia Kimball
February 23, 2026 AT 21:50I'm a nurse and this made me cry. Not because it's sad-but because it's true. I’ve seen patients who waited months to speak up about pain because they didn’t want to be 'a burden.' Then we started using the scale, and one woman said, 'I didn’t know I was allowed to say I was at an 8.' That one sentence changed everything. We started giving her gabapentin, then radiation, then a massage therapist came in once a week. She danced with her husband two weeks before she passed. That’s what this is for. Not statistics. Not ladders. Just moments.
Kapil Verma
February 23, 2026 AT 23:42India has been doing this right for decades. We don’t need your Western bureaucracy. Our Ayurvedic pain clinics use ashwagandha, turmeric, and yoga breathing to manage cancer pain better than your opioids. You think morphine is science? We have been treating pain with plant-based wisdom since before your ancestors invented the wheel. Your 'ladder' is just colonial thinking dressed in white coats. India’s palliative care model is more humane, cheaper, and culturally rooted. You should be learning from us, not lecturing us.
Michael Page
February 25, 2026 AT 03:26It's interesting how the article frames pain as a problem to be solved. But what if pain isn't meant to be eliminated? What if it's a signal-a reminder that we are still here, still feeling, still alive? The more we try to numb it, the more we distance ourselves from the raw truth of mortality. Maybe the real breakthrough isn't a new drug, but the courage to sit with discomfort without rushing to fix it. Not all suffering needs curing. Sometimes it just needs witnessing.
Mandeep Singh
February 26, 2026 AT 01:09Let me tell you something you won't hear in your fancy American hospitals. In India, we don't wait for 'early intervention.' We treat pain aggressively from day one. We use morphine like it's water. We don't have time for your 'step-by-step ladder' when someone is screaming at 3 a.m. because their spine is collapsing. And you think insurance is a problem? Try getting a single dose of fentanyl patch in a rural village with no electricity, no refrigeration, and a doctor who hasn't seen a cancer patient in six months. This whole post reads like a tourist brochure. Real pain doesn't care about your 0-10 scale. It doesn't care if you're 'dignified.' It just hurts. And if you're not giving enough medicine, you're not helping. You're just being polite.
Betty Kirby
February 26, 2026 AT 19:33So we're supposed to believe that giving someone morphine is 'fighting for quality'? What about the 12-year-old whose dad became addicted after his cancer diagnosis? What about the family that lost everything paying for a $3,000 nerve block that insurance denied? This isn't compassion-it's corporate healthcare selling you a dream wrapped in clinical jargon. You call it 'dignity.' I call it a PR campaign. And the people who actually suffer? They're still waiting for someone to listen.