Every year, over 30 million people worldwide take NSAIDs for pain, swelling, or fever. These drugs - ibuprofen, naproxen, celecoxib - are everywhere. You can buy them over the counter. Your doctor prescribes them for arthritis. But for all their usefulness, they carry hidden dangers that don’t show up until it’s too late. The real problem isn’t just stomach pain. It’s bleeding you can’t see. Kidney damage that creeps up slowly. And most people have no idea they’re at risk.
How NSAIDs Hurt Your Stomach - Even When You Feel Fine
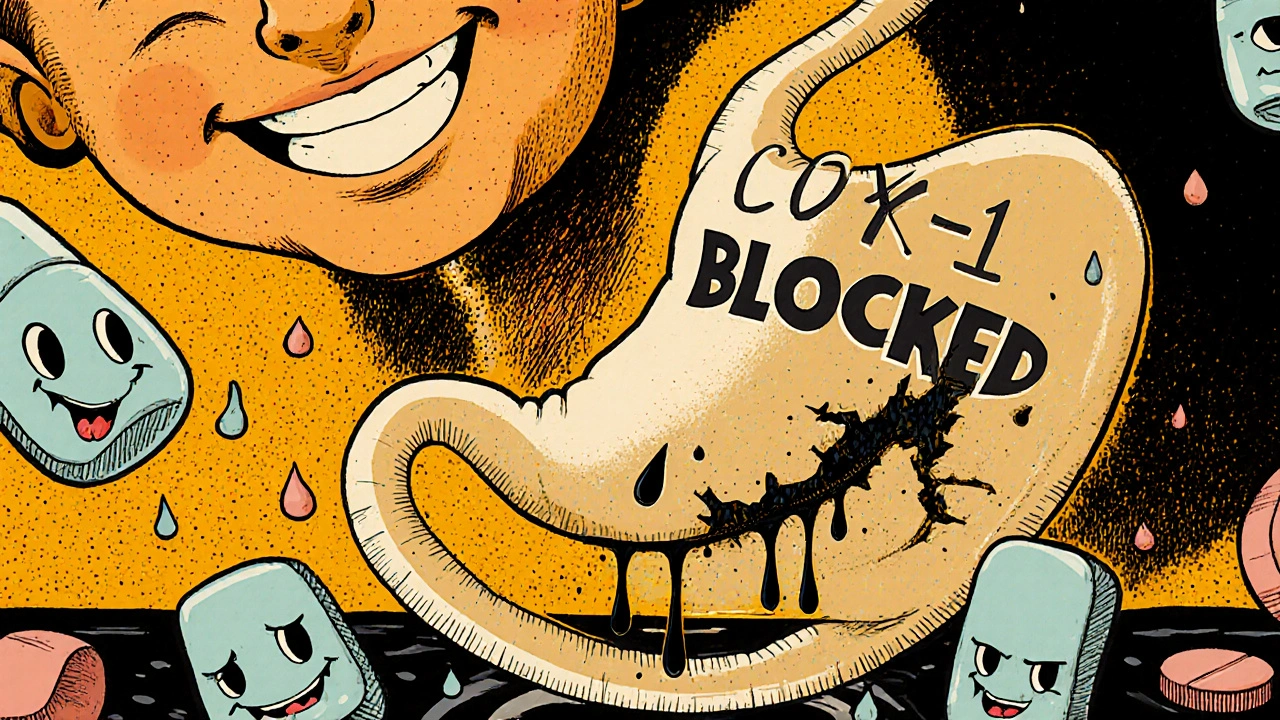
NSAIDs work by blocking enzymes called COX-1 and COX-2. That’s how they reduce pain and inflammation. But COX-1 also helps protect your stomach lining. When you block it, your stomach loses its natural defense. The result? Ulcers, bleeding, even perforations. And here’s the scary part: half of all NSAID-related stomach damage happens without warning symptoms. You don’t feel burning. You don’t notice black stools. Then, suddenly, you’re in the ER with low blood pressure and a hemoglobin level that’s crashed.Studies show 10% to 50% of people who take NSAIDs long-term develop some form of stomach lining damage. About 15% end up with peptic ulcers. And every year in the U.S. alone, NSAIDs cause over 100,000 hospitalizations and 16,500 deaths. Most of those deaths happen because the damage was silent until it wasn’t.
It’s not just the upper GI tract. NSAIDs also wreck the small intestine. They cause inflammation, ulcers, and bleeding down there too. Unlike stomach ulcers, there’s no reliable way to prevent or treat this lower GI damage. No magic pill. No proven supplement. The only real fix is stopping the NSAID - and even then, healing can take months.
Kidney Damage Is Quiet, But Deadly
Your kidneys rely on prostaglandins to keep blood flowing properly. NSAIDs block those prostaglandins. In healthy people, that’s usually fine. But if you’re dehydrated, older than 65, or already have kidney issues, it’s a different story. Your kidneys start to struggle. Blood pressure drops inside the kidney filters. Glomerular filtration rate (GFR) falls. Creatinine rises.Acute kidney injury from NSAIDs happens in 1% to 5% of users. That might sound low, but when you’re talking about millions of users, that’s tens of thousands of people each year. Chronic use? That’s when you see papillary necrosis - tissue death in the kidney’s inner layer - and interstitial nephritis. Both can lead to permanent kidney damage. The FDA now requires a boxed warning on all prescription NSAIDs for kidney risks in patients over 65. That’s not a suggestion. It’s a red flag.
And here’s what most patients don’t realize: if you’re taking NSAIDs daily and never get your kidney function checked, you’re flying blind. A simple blood test for creatinine and BUN can catch trouble early. But only 52% of NSAID users have this test done within 90 days of starting, according to Medicare data. That’s not monitoring. That’s negligence.
Not All NSAIDs Are Created Equal
If you’re going to take one, you need to know which one carries the least risk - and which ones are worst.Non-selective NSAIDs like ibuprofen and naproxen hit both COX-1 and COX-2. That means more stomach damage. Naproxen increases the risk of upper GI bleeding by 4.2 times compared to non-users. Ibuprofen? It’s 2.7 times more likely to cause ulcers than celecoxib.
COX-2 inhibitors like celecoxib were designed to be safer for the stomach. And they are - but only partially. They cut GI bleeding risk by about half compared to naproxen. But they still carry kidney risks. And they’re not safe for people with heart disease. In fact, patients on blood thinners who take any NSAID double their risk of GI bleeding and raise their chance of heart attack or stroke by 40%.
Here’s a hard truth: there’s no “safe” NSAID. There’s only “less dangerous.” And even celecoxib isn’t risk-free. A 2022 patient survey found 22% of celecoxib users reported leg swelling - a sign of fluid retention and possible kidney strain.
Who’s at Highest Risk?
Not everyone needs the same level of caution. But if you fall into any of these categories, you’re in the danger zone:- Age 65 or older
- History of peptic ulcer or GI bleeding
- Taking blood thinners like warfarin or apixaban
- Using corticosteroids (like prednisone)
- Having chronic kidney disease (eGFR below 60)
- Diagnosed with heart failure or high blood pressure
- Taking SSRIs (antidepressants like sertraline or fluoxetine)
Each of these adds points to your risk score. The American College of Gastroenterology has a simple calculator: age over 65 = 2 points, prior ulcer = 3 points, anticoagulants = 2 points, steroids = 1 point. Four or more points? You’re high risk. You need a plan - not just a prescription.

Monitoring: What You Need to Track
If you’re on NSAIDs long-term, you need regular checks. Not “when you feel bad.” Regular. Scheduled. Non-negotiable.Here’s what your doctor should be testing - and how often:
- Serum creatinine and BUN: Check within 30 days of starting, then every 3-6 months. If you’re over 70 or have kidney disease, check every 3 months.
- Complete blood count (CBC): Look for low hemoglobin. That’s a sign of slow, hidden bleeding. Do this every 6 months if you’re high risk.
- Fecal occult blood test (FOBT): The new point-of-care FIT tests (launched in 2024) are 92% accurate at spotting hidden blood in stool. Do this every 6 months if you’re on NSAIDs for more than 3 months.
- Blood pressure: NSAIDs can raise BP. Monitor monthly if you’re hypertensive.
And don’t assume your doctor is doing this. Ask. Write it down. Bring a printed checklist to your appointment. If they don’t test, find someone who will.
What About PPIs? Are They the Answer?
Proton pump inhibitors (PPIs) like omeprazole are often prescribed with NSAIDs to protect the stomach. And yes - they reduce ulcer risk by 70% to 90%. But here’s what no one tells you: PPIs aren’t harmless.Studies show that combining NSAIDs and PPIs for 4 to 12 months increases your risk of microscopic colitis - a chronic, inflammatory bowel condition - by more than six times. That’s not protection. That’s swapping one problem for another.
And PPIs don’t help your lower GI tract. They don’t stop intestinal ulcers. They don’t protect your kidneys. They’re a partial fix for a full-system problem.
Dr. Kenneth W. Mahaffey calls it the “therapeutic paradox”: we use PPIs to fix one risk, and end up creating new ones. The real solution isn’t more pills. It’s less NSAID use.
What Should You Do Instead?
The best way to avoid NSAID complications? Don’t take them unless you absolutely have to.Here’s what works better:
- Physical therapy: For osteoarthritis and back pain, PT is as effective as NSAIDs - with zero side effects.
- Topical NSAIDs: Gels and patches deliver pain relief with 90% less systemic absorption. Much safer for stomach and kidneys.
- Acetaminophen: For simple pain, it’s the first-line choice. No GI or kidney risk (though liver risk exists at high doses).
- Weight loss and movement: Losing just 5% of body weight cuts knee osteoarthritis pain by 50%. Movement is medicine.
- Heat, cold, TENS units: Simple, safe, and often effective.
If you must use NSAIDs, use the lowest dose for the shortest time possible. Every extra week of use increases your complication risk by 3% to 5%. That’s not a small number. That’s a ticking clock.

The Future: New Options on the Horizon
There’s some hope on the horizon. In 2023, the FDA approved naproxcinod - a new NSAID that releases nitric oxide, which helps protect blood vessels and the stomach lining. In trials, it caused 58% fewer ulcers than regular naproxen.Also in 2024, a new fecal immunochemical test (FIT) became available - designed specifically for NSAID users. It’s more accurate than older stool tests and can be done at home.
But these are still new. They’re not widely available. And they don’t solve the core problem: we’re overprescribing NSAIDs like they’re candy.
Experts predict that without better strategies to protect the lower GI tract, NSAID-related hospitalizations will rise 18% over the next decade. That’s not inevitable. It’s preventable - if we stop treating pain with pills and start treating it with care.
Frequently Asked Questions
Can I take NSAIDs if I have high blood pressure?
NSAIDs can raise blood pressure and interfere with hypertension medications like ACE inhibitors or diuretics. If you have high blood pressure, avoid NSAIDs unless your doctor says it’s safe. Use acetaminophen or topical pain relievers instead. Always check your BP regularly if you must use NSAIDs.
How long is it safe to take ibuprofen daily?
For most people, daily ibuprofen should not exceed 10 days without medical supervision. Long-term daily use - even at low doses - increases the risk of stomach ulcers, kidney damage, and heart problems. If you need pain relief for more than 10 days, talk to your doctor about alternatives.
Are OTC NSAIDs safer than prescription ones?
No. The same risks apply whether you buy NSAIDs over the counter or get them by prescription. Many people think OTC means safe, but taking high doses of ibuprofen daily for months is just as dangerous as taking a prescription-strength dose. The dose and duration matter more than the label.
What should I do if I notice black stools or dark urine?
Black, tarry stools are a sign of upper GI bleeding. Dark urine may indicate kidney damage or muscle breakdown. Stop taking NSAIDs immediately and seek medical attention. Do not wait for symptoms to worsen. These are medical emergencies.
Can I take NSAIDs if I’ve had a heart attack?
No. If you’ve had a heart attack, avoid all NSAIDs unless your cardiologist specifically approves one. Even short-term use increases your risk of another heart attack, stroke, or death. Acetaminophen is the preferred pain reliever in this group - but always check with your doctor first.
Is it safe to take NSAIDs with antidepressants like SSRIs?
No. Combining NSAIDs with SSRIs increases your risk of GI bleeding by more than three times. This combination is especially dangerous for older adults. If you’re on an SSRI and need pain relief, ask your doctor about alternatives like topical NSAIDs, acetaminophen, or physical therapy.
Next Steps for Safe Pain Management
If you’re on NSAIDs right now, here’s what to do:- Write down every NSAID you’ve taken in the last 6 months - including OTC brands and doses.
- Check your last blood pressure, creatinine, and hemoglobin results. If you don’t know them, call your doctor’s office.
- Ask your doctor: “Am I high risk? Do I need a GI or kidney check?”
- Start exploring non-drug options: physical therapy, weight management, heat therapy, or topical gels.
- If you’ve been on NSAIDs for more than 3 months, get a fecal occult blood test - even if you feel fine.
NSAIDs aren’t evil. They help millions. But they’re not harmless. The key isn’t fear. It’s awareness. If you’re taking them regularly, you owe it to yourself to know the risks - and how to protect yourself.

 Health and Wellness
Health and Wellness
Matthew Higgins
November 29, 2025 AT 22:04I’ve been taking ibuprofen for my back pain for years. Never thought twice about it until I read this. Now I’m scared to even look at my medicine cabinet. 😅
Brandy Johnson
November 30, 2025 AT 04:37It is imperative to recognize that the systemic pharmacological disruption induced by non-selective cyclooxygenase inhibition constitutes a preventable public health crisis of monumental proportions. The absence of mandatory renal and hematologic surveillance protocols for over-the-counter NSAID consumption is a regulatory failure of staggering magnitude.
Peter Axelberg
December 2, 2025 AT 04:00Man, I used to think NSAIDs were just like aspirin - harmless little painkillers. Turns out they’re like tiny little landmines in your gut and kidneys. I’ve been on naproxen for my arthritis for 8 years. I never got my blood work done. Now I’m freaked out. I’m gonna schedule a checkup this week. No more pretending it’s fine.
And don’t even get me started on PPIs. I’ve been on omeprazole for three years because of my NSAIDs. My doctor said it was fine. Now I find out it might be giving me colon inflammation? That’s wild. I feel like I’ve been played.
My grandma took ibuprofen every day for her knees. She ended up in the hospital with a GI bleed. No warning. No symptoms. Just… gone. I didn’t realize how many people this is quietly killing.
Topical NSAIDs? I didn’t even know those existed. I’m gonna try the gel. Way better than swallowing a pill every day. And PT? I’ve been avoiding it because it’s a hassle. But if it’s just as good as the pills and doesn’t wreck my insides… yeah. I’m in.
Also, the part about SSRIs and NSAIDs? I’m on sertraline. I didn’t know that combo was a death sentence. I’m gonna talk to my doctor tomorrow. Seriously. This article changed my life.
I used to think people who complained about side effects were just whiny. Now I get it. These drugs aren’t safe. They’re just… available. And that’s the problem.
My cousin died at 58 from an NSAID-induced ulcer. He was healthy. He took Advil for his headaches. No history of ulcers. No warning. Just… one day, he collapsed. This isn’t theoretical. This is real. And we’re all just walking around like it’s normal.
Why isn’t there a warning label on every OTC bottle that says: ‘May silently kill your kidneys and stomach’? Because the drug companies don’t want you to stop buying. That’s the truth.
I’m done. I’m switching to acetaminophen. I’m getting my creatinine checked. I’m doing PT. And I’m telling everyone I know. This needs to be common knowledge.
I’m not trying to scare anyone. But if this post saves one person from ending up in the ER with a bleeding ulcer… it’s worth it.
Monica Lindsey
December 3, 2025 AT 06:48Anyone who takes NSAIDs daily without monitoring is either ignorant or reckless. There is no middle ground.
Jennifer Wang
December 3, 2025 AT 12:34As a clinical pharmacist, I can confirm the data presented here is accurate and underappreciated. The 2024 FIT test for occult blood in NSAID users is a significant advancement - it’s non-invasive, highly sensitive, and should be standard of care for anyone on chronic NSAID therapy. I routinely recommend it to patients over 50 on long-term NSAIDs. Additionally, the risk of acute kidney injury is highest within the first 30 days of initiation - a critical window often missed in primary care. Always check creatinine before and within 30 days of starting NSAIDs, regardless of perceived risk.
stephen idiado
December 4, 2025 AT 12:38COX-2 inhibition is a pharmacological fallacy. The prostaglandin axis is not modular. You cannot selectively target inflammation without systemic collateral damage. This is biochemistry 101 - yet the FDA approved celecoxib as a ‘safer’ option. Corporate influence, not science.
Subhash Singh
December 5, 2025 AT 01:08This is an exceptionally well-researched piece. I am from India, where NSAIDs are sold over the counter without any prescription or counseling. The prevalence of silent GI bleeding and NSAID-induced nephropathy is alarmingly high, especially among elderly patients with arthritis. I have personally witnessed three cases in my community where patients presented with hemodynamic collapse due to unrecognized GI hemorrhage. Public health education on this issue is critically lacking.
Geoff Heredia
December 5, 2025 AT 13:06They don’t want you to know this. The NSAID industry is part of a bigger system - the pharmaceutical complex that profits from chronic illness. PPIs? Designed to sell more pills. The ‘monitoring’ advice? A loophole to keep you dependent. They’re not trying to protect you. They’re trying to keep you buying. And now they’re pushing ‘safer’ NSAIDs that cost 10x more. Wake up.
Tina Dinh
December 6, 2025 AT 16:06OMG this is SO important!! 🙏 I just started taking naproxen for my knee and I had NO IDEA 😱 I’m booking a blood test TODAY and switching to topical gel! Also, PT is now my new best friend 💪🔥 #NSAIDAwareness #PainManagement
Andrew Keh
December 7, 2025 AT 19:25This is a very clear and necessary warning. I’ve been taking ibuprofen for years without thinking about the risks. I’ll be more careful from now on. Thank you for sharing this.
gerardo beaudoin
December 7, 2025 AT 19:28Good stuff. I’ve been on celecoxib for 2 years. My doctor never mentioned the kidney risk or the need for blood tests. I’m gonna ask for my labs next visit. Also, I’ve been using the topical NSAID gel for my shoulder - way better than pills. No stomach upset at all.
tushar makwana
December 8, 2025 AT 06:25i never knew about the small intestine thing… my uncle had to get surgery because of it and he was only 55. he took ibuprofen for his back every day. no symptoms. just one day he was in pain and then boom. this is scary. i’m gonna stop taking it for headaches now. maybe try heat pack or something.
Richard Thomas
December 9, 2025 AT 19:31The notion that NSAID-related mortality is somehow ‘preventable’ through patient education is a gross misrepresentation of the structural realities of modern healthcare delivery. The onus of vigilance cannot be placed on laypersons who are systematically deprived of accessible, affordable, and timely clinical oversight. The burden of responsibility lies not with the consumer, but with the institutional failure to enforce mandatory biomonitoring protocols - a failure that is both systemic and intentional.
Scott Collard
December 10, 2025 AT 17:37You’re all missing the point. NSAIDs are just one symptom. The real problem is that we’ve turned every ache into a crisis that needs a chemical fix. We’ve lost the ability to sit with discomfort. That’s the real epidemic.