
Mycophenolate Side Effect Management Calculator
Find Your Best Management Strategy
Answer a few quick questions to get personalized recommendations for managing mycophenolate side effects based on clinical evidence.
Current Medication
Primary Symptom
Symptom Severity
Current Dose
Personalized Management Plan
Key Evidence-Based Strategies
When you're taking mycophenolate after a transplant or for an autoimmune condition, the last thing you want is to feel sick to your stomach or have constant diarrhea. These aren't just minor annoyances-they can make you miss doses, skip meals, or even stop taking the medication entirely. And if you stop, your body might start rejecting your new organ or flare up your disease. About one in two people on mycophenolate experience nausea or diarrhea, especially in the first few months. The good news? There are clear, proven ways to manage these side effects without giving up the drug.
Why Mycophenolate Makes You Feel Sick
Mycophenolate-sold as CellCept or Myfortic-works by slowing down your immune system. It blocks a key enzyme called IMPDH, which immune cells need to multiply. That’s why it helps prevent organ rejection. But that same enzyme is also important in the lining of your gut. When it’s suppressed, the cells that keep your intestines healthy get damaged. This leads to inflammation, poor absorption, and irritation. That’s why nausea and diarrhea are so common. In clinical trials, 31% of patients had nausea, and nearly 30% had diarrhea. For some, it’s mild. For others, it’s debilitating enough to force them off the drug.
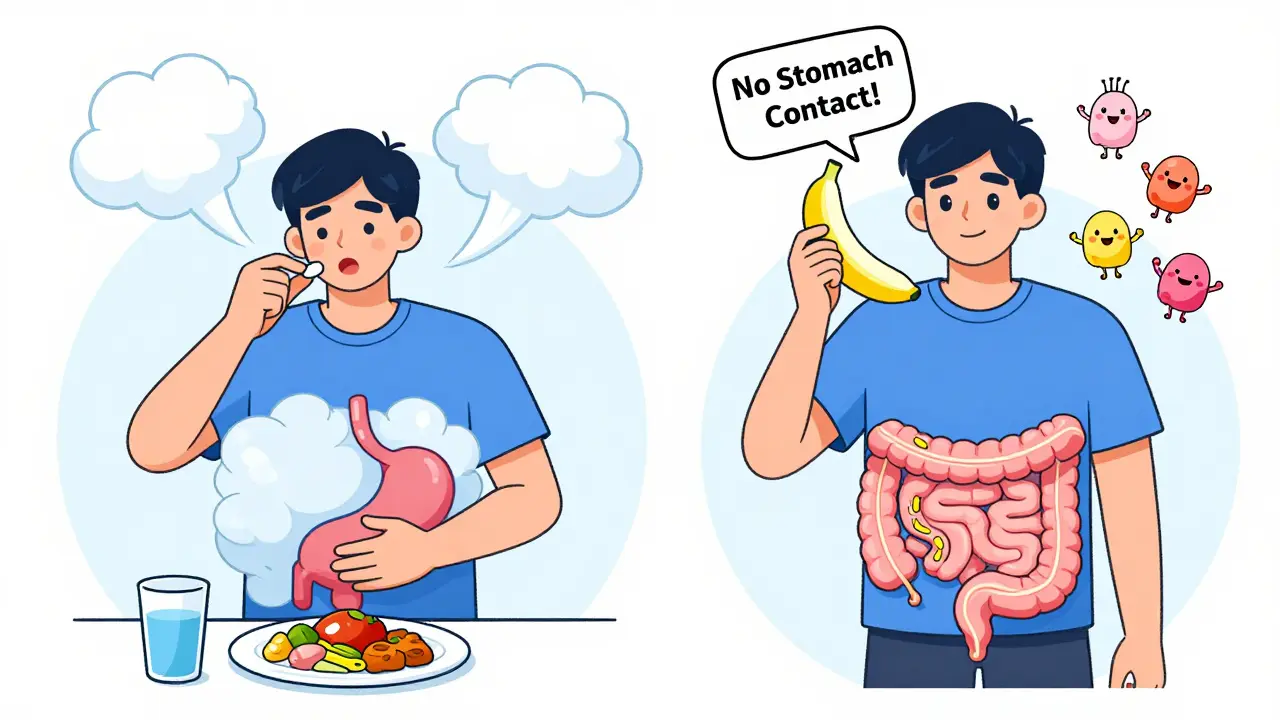
Not everyone reacts the same way. People who take mycophenolate mofetil (CellCept) are more likely to have upper GI issues like nausea and vomiting because the tablet dissolves in the stomach. Mycophenolate sodium (Myfortic), with its enteric coating, is designed to pass through the stomach and dissolve in the small intestine. That helps reduce nausea, but diarrhea can still happen.
Dose Reduction Works Better Than You Think
Many patients and even some doctors assume that lowering the dose means the drug won’t work. That’s not true. A 2021 study from Johns Hopkins followed 87 transplant patients with moderate to severe diarrhea. When their dose was reduced by one-third-for example, from 1,000 mg twice daily to 667 mg twice daily-78% saw their symptoms disappear within 72 hours. Their mycophenolic acid (MPA) levels stayed within the safe and effective range: 1 to 3.5 μg/mL. This is critical. You don’t need the highest possible dose. You need the lowest dose that still prevents rejection.
Doctors often hesitate to reduce the dose because they fear rejection. But data shows that rejection rates don’t increase when doses are lowered appropriately. In fact, patients who stick with a reduced dose are more likely to stay on the medication long-term. If you’re struggling with side effects, ask your pharmacist or transplant team to check your MPA trough level. It’s a simple blood test. If it’s above 3.5 μg/mL, you’re likely getting more than you need.
Switching from CellCept to Myfortic Can Help
If you’re on mycophenolate mofetil (CellCept) and you’re getting nauseous, switching to the enteric-coated version-mycophenolate sodium (Myfortic)-is one of the most effective moves you can make. A 2022 trial with 120 kidney transplant patients found that 65% of those who switched had significant improvement in nausea and vomiting. Diarrhea didn’t always go away, but it became more manageable. The coating delays release until the drug reaches the small intestine, avoiding direct contact with the stomach lining.
It’s not a magic fix. About one-third of patients still have diarrhea after switching. But for those with nausea as the main problem, it’s often enough to make the difference between sticking with the drug and quitting it. Your doctor can easily switch your prescription. Insurance usually covers it because the total cost is similar. And if you’re on generic mycophenolate mofetil, switching to generic Myfortic is just as effective.
Timing Matters: When You Take It Changes Everything
The Cleveland Clinic updated its guidelines in 2023: take mycophenolate on an empty stomach-either one hour before or two hours after eating. That’s because food, especially fatty meals, can reduce absorption and cause more GI upset. But here’s the twist: if you’re throwing up or nauseous, taking it with a small amount of food can help.
A Reddit thread from March 2024 with 287 comments from transplant patients showed that 62% of those who took their pill with a spoonful of applesauce or plain yogurt reported less nausea. Applesauce is low-fat, easy to digest, and doesn’t interfere with absorption like greasy food does. Other common tips: take it with a banana, toast, or a few crackers. Don’t take it with orange juice or milk-those can affect how the drug is absorbed.
Splitting your dose also helps. Instead of two big pills, take one in the morning and one in the evening, but make sure you’re still giving your body at least 12 hours between doses. Some patients find taking one dose at bedtime helps, because nausea often fades while they sleep.
Probiotics Aren’t Just for Yogurt
Research on probiotics for mycophenolate-induced diarrhea is still emerging, but real-world evidence is strong. A 2023 survey of 33 patients found that 49% who took Lactobacillus GG (a specific strain found in Culturelle or Bio-K+) noticed fewer bowel movements and less urgency. Another study from the University of Michigan showed that patients using probiotics for at least four weeks had a 30% reduction in diarrhea severity.
Not all probiotics work. Stick to strains with evidence: Lactobacillus GG, Bifidobacterium infantis, or Saccharomyces boulardii. Avoid multi-strain blends unless they’re specifically studied for transplant patients. Take them at least two hours apart from your mycophenolate to avoid interference. Probiotics won’t fix everything, but they can be a simple, low-risk addition.
When It’s More Than Just Upset Stomach
If your diarrhea lasts more than seven days, especially if it’s bloody, accompanied by cramps, fever, or weight loss, don’t wait. You could have mycophenolate-induced colitis-a rare but serious inflammation of the colon. It’s not an infection, but it looks like one. The only way to know for sure is a colonoscopy with biopsy. Under the microscope, doctors look for apoptosis (cell death) in the lining of your intestines, which is a telltale sign of mycophenolate damage.
It’s easy to mistake this for a C. diff infection or CMV, which are common in transplant patients. That’s why guidelines now recommend testing for infections first, then considering mycophenolate toxicity if tests come back negative. If it’s confirmed, you’ll need to stop the drug completely for a few weeks. Then, your team may try rechallenging you with a much lower dose. But be warned: 42% of people who rechallenge have symptoms return.
What to Do If You Can’t Tolerate It
Some people just can’t handle mycophenolate, no matter what adjustments are made. About 14% of transplant patients permanently stop it within the first year. If you’re one of them, there are alternatives. Azathioprine is the most common, but it’s less effective and has its own side effects. Leflunomide is newer and shows promise in early studies-it’s been used successfully in patients who failed mycophenolate. It’s not FDA-approved for all transplant types yet, but many centers use it off-label.
There’s also a new extended-release version of mycophenolate (MPA-ER) that got FDA approval in March 2023. In trials, it cut diarrhea rates by 37% compared to the old immediate-release version. It’s not widely available yet, but if you’re struggling, ask if you’re eligible for it.

What Not to Do
- Don’t skip doses to avoid side effects. This increases rejection risk.
- Don’t take over-the-counter anti-diarrhea meds like loperamide (Imodium) without talking to your doctor. They can mask symptoms and delay diagnosis of serious conditions.
- Don’t assume your symptoms will go away on their own. Most improve within 3-6 months, but some need active management.
- Don’t ignore weight loss or dehydration. These are red flags.
Real Patient Strategies That Work
From real patient experiences, here’s what’s working:
- Applesauce trick: 62% of 48 respondents on Reddit said it cut nausea.
- Split doses: 57% found taking one pill in the morning and one at night helped.
- Probiotics: 49% of users reported fewer bowel movements with Lactobacillus GG.
- Hydration: Drinking 2-3 liters of water daily helped 71% manage diarrhea symptoms.
- Low-FODMAP diet: Avoiding onions, garlic, beans, and artificial sweeteners helped 41% reduce bloating and urgency.
These aren’t guesses. These are patterns from hundreds of transplant patients who’ve lived through this. You don’t have to suffer in silence. Talk to your transplant team. Ask for a pharmacist consult. They’ve seen this before.
Final Thoughts
Mycophenolate isn’t perfect, but it’s still the most effective drug for preventing rejection. The GI side effects are common, but they’re not inevitable. You have options: reduce the dose, switch formulations, change when you take it, add probiotics, or try a newer version. The goal isn’t to eliminate side effects completely-it’s to find the balance where you stay healthy without feeling miserable. Most people find that balance. You can too.

 Health and Wellness
Health and Wellness
Sarah B
February 7, 2026 AT 18:45Tola Adedipe
February 8, 2026 AT 16:32Eric Knobelspiesse
February 10, 2026 AT 12:45also i took mine with orange juice once. turned out okay. who's to say what's right?
Mark Harris
February 12, 2026 AT 02:16Marcus Jackson
February 12, 2026 AT 17:28I've been on this for 5 years. I don't trust any of this. I take it with coffee. Works fine.
Natasha Bhala
February 13, 2026 AT 14:57ps. applesauce is magic
Jesse Lord
February 14, 2026 AT 06:20You're not broken. You're adapting.
Catherine Wybourne
February 14, 2026 AT 12:32I switched to Myfortic. Still had diarrhea. So I started a low-FODMAP diet. No onions. No garlic. No avocado. My partner thinks I'm insane. I think he's just jealous he doesn't have to do this.
Also, probiotics. Not magic. Just... less awful.
Paula Sa
February 15, 2026 AT 14:10Dose reduction isn't surrender. It's wisdom. And applesauce? That's not a hack. That's love. Your body just needed a gentle hand.
Amit Jain
February 16, 2026 AT 22:32This whole system is rigged. They want you hooked. Don't be a sheep.
Heather Burrows
February 17, 2026 AT 20:29We're told to 'manage' it. But what if it's not meant to be managed? What if it's a sign?
Maybe we should stop pretending we can outsmart biology.
Gouris Patnaik
February 19, 2026 AT 13:50i take mine with chai. and i don't care if it's not 'evidence-based'. my body knows. and i'm still here. 7 years. no rejection. no drama. just chai. and faith.