
Every year, tens of thousands of children end up in emergency rooms because of a simple mistake: the wrong dose of medicine. It’s not because parents are careless. It’s because the system is set up to fail them - and often, the staff under pressure are too.
In pediatric emergencies, medication errors happen more than twice as often as in adults. One study found that 31% of pediatric medication orders contain some kind of error, compared to just 13% in adults. That’s not a small gap. That’s a crisis.
Why Kids Are at Higher Risk
Adults usually get pills with fixed doses - one tablet, twice a day. Kids don’t. Their doses are calculated by weight: milligrams per kilogram. That means every child, even those who look similar, needs a different amount. A 10kg toddler needs less than half the dose of a 22kg 5-year-old. One wrong decimal, one misread number, and you’ve given a 10x overdose.
Most pediatric meds come as liquids. That sounds safer - easier to swallow, easier to adjust - but it’s where most mistakes happen. Parents use kitchen spoons, syringes without markings, or confuse milligrams (mg) with milliliters (mL). One parent gave 5mL of children’s Tylenol thinking it was the same as infant concentrate. It wasn’t. The concentration was different. The child ended up in the ER with liver damage.
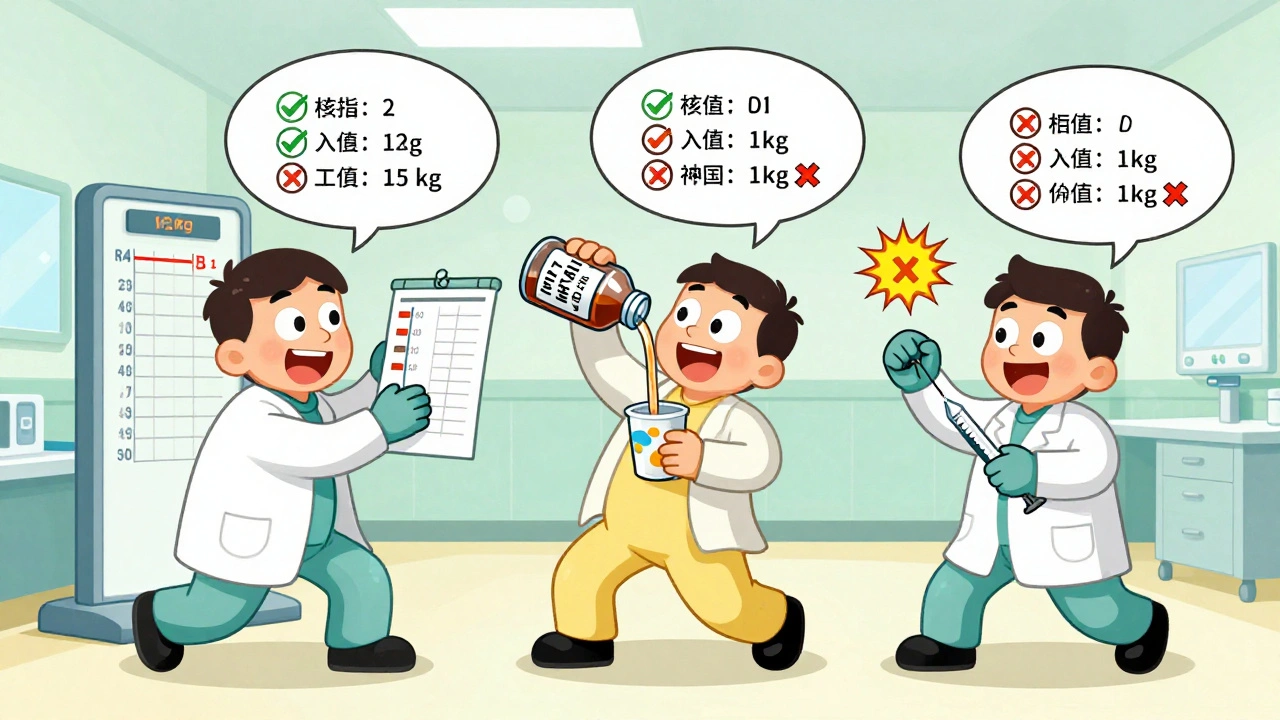
Studies show 60% to 80% of home dosing errors involve liquid medications. And it’s not just parents. Even trained staff in busy ERs misread weights, skip double-checks, or mishear verbal orders. One study found that 10% to 31% of errors came from incorrect weight measurements. If the scale says 15kg but the chart says 12kg, the dose is already wrong before it’s even drawn up.
The Most Common Mistakes - and What They Cost
Here’s what the data tells us about the top errors in pediatric emergency settings:
- Wrong dose - 13% of all pediatric medication errors
- Wrong medication - 4%
- Wrong time or rate - 3%
- Wrong route - 1%
And the consequences? One in eight of these errors causes real harm. That’s 13%. Another 47% reach the child but don’t cause injury - lucky breaks. The rest are caught before they get to the patient. But that’s still 31% of all pediatric med orders having some kind of problem.
At home, the numbers are even scarier. One study found that 1 in 10 parents of children with leukemia made dosing mistakes with oral chemotherapy. That’s not a typo. That’s a life-threatening error. And it’s not rare.
Costs add up fast. Around 63,000 children visit the ER each year because of home medication mistakes. That’s $28 million in emergency care costs - all from avoidable errors.
Case Lessons: What Actually Happened
Let’s look at real cases - not hypotheticals.
Case 1: A 2-year-old with a fever. Mom gives 5mL of children’s acetaminophen. The child weighs 10kg. The correct dose is 10mg/kg = 100mg total. But the liquid is 160mg per 5mL. So 5mL = 160mg. That’s 60% over the safe dose. Not fatal - but enough to stress the liver. The child was monitored overnight. No long-term damage. But it could have been worse.
Case 2: A mother gives her 3-year-old ibuprofen because she thought the bottle said “5mL for under 12kg.” She didn’t see the small print: “For children 12-23 months.” Her child was 36 months. The dose was double what it should’ve been. She called the pediatrician after noticing the child was unusually sleepy. They caught it before harm occurred.
Case 3: A father gives his 8kg baby 2.5mL of amoxicillin twice a day. The prescription said 2.5mL once a day. He thought “twice a day” meant “double the volume.” He didn’t understand the difference between frequency and volume. The child developed diarrhea and vomiting. ER visit. Diagnosis: antibiotic overdose.
These aren’t outliers. They’re routine.
Who’s Most at Risk?
It’s not about income. It’s about access, language, and literacy.
Parents with low health literacy make 2.3 times more dosing errors than those with higher literacy. Non-English speakers? Their error rate jumps to 45%. Spanish-speaking families in one study had 32% higher error rates than English-speaking ones - even when given translated instructions.
Children on Medicaid are 27% more likely to have a medication error than those with private insurance. Why? Fewer follow-ups. Less pharmacy support. Less time with providers. The system doesn’t catch them before they slip through.
What Works: Proven Fixes
There’s good news. We know what reduces these errors.
1. Teach-back method - After giving instructions, ask the parent to explain it back in their own words. Don’t say “Do you understand?” Say “Can you show me how you’ll give this at home?” This simple trick cuts errors by 25%.
2. Standardized measuring tools - Give parents a syringe or dosing cup with clear markings. No more teaspoons. No more cups. A 2024 study found that using these tools reduces errors by 35% to 45%.
3. Pictograms and simple instructions - Instead of “Give 10mg/kg every 6 hours,” use a picture: a child, a syringe, a clock showing 6-hour intervals. One hospital called this the MEDS intervention. It cut dosing errors from 64.7% down to 49.2% - and kept them low even after the program ended.
4. Double-checks in the ER - At Nationwide Children’s Hospital, every pediatric dose is verified by a second clinician and a pharmacist. Result? An 85% drop in harmful medication events. It’s not magic. It’s discipline.
5. EMR systems with pediatric dosing calculators - Sixty-eight percent of children’s hospitals now use EMRs that auto-calculate doses based on weight. But most general ERs don’t. That’s a dangerous gap. A kid taken to a community hospital might get a dose calculated by hand - on a sticky note - while the one at the children’s hospital gets it done by a system with built-in safety alerts.

What’s Still Broken
We have tools. We have data. We have proof that change works.
But we don’t have consistent standards. No one tracks outpatient pediatric medication errors the way they track hospital falls or infections. There’s no national reporting system. No mandatory metrics. The American Academy of Pediatrics wants to fix that by 2025 - but right now, we’re flying blind.
Pharmacies don’t always label pediatric meds clearly. Some still use “per teaspoon” instead of “per mL.” Some bottles have tiny print. Some don’t list concentration at all.
And the biggest problem? We assume parents know how to measure. We don’t teach them. We hand them a syringe and walk away.
What You Can Do - Right Now
If you’re a parent:
- Always ask: “Is this dose based on my child’s weight?”
- Use only the measuring tool that comes with the medicine. Never a kitchen spoon.
- Take a photo of the prescription label before leaving the ER or pharmacy.
- Ask: “Can you show me how to use this syringe?”
- If you’re unsure - call your pediatrician. Don’t guess.
If you’re a clinician:
- Always confirm weight - don’t trust the chart. Weigh the child if possible.
- Use a double-check system for all high-risk meds (like morphine, insulin, chemotherapy).
- Use pictograms. Always.
- Teach-back. Every time.
- Advocate for pediatric-specific EMR tools in your hospital.
It’s Not About Blame
This isn’t about bad parents or lazy nurses. It’s about a system that hasn’t caught up to the reality of pediatric care.
Kids aren’t small adults. Their bodies process drugs differently. Their doses are precise. Their caregivers are often exhausted, stressed, and under-informed.
But we can fix this. We’ve already seen it work - in hospitals that use checklists, in clinics that give syringes, in families who get clear pictures and simple words.
One wrong dose can change a child’s life. But one simple step - asking them to show you how they’ll give the medicine - can stop it before it happens.
Why are pediatric medication errors more common than adult ones?
Pediatric doses are based on weight (mg/kg), not fixed amounts like in adults. This requires calculations for every child, increasing the chance of math errors. Most pediatric meds are liquids, which are harder to measure accurately. Parents often confuse milligrams (mg) with milliliters (mL), and many use kitchen spoons instead of proper dosing tools. Emergency settings add pressure, time limits, and verbal orders - all of which raise the risk.
What’s the most common type of pediatric medication error?
Wrong dose is the most common, accounting for 13% of all pediatric medication errors. This usually happens because of incorrect weight measurement, miscalculating mg/kg, or confusing concentration levels in liquid medications - like giving 5mL of a stronger infant formula when the child needs the weaker children’s version.
How can parents avoid giving the wrong dose at home?
Always use the dosing syringe or cup that comes with the medicine - never a kitchen spoon. Double-check the weight-based dose with your child’s current weight. Ask the provider to show you how to use the syringe. Take a photo of the label. Use the teach-back method: repeat the instructions out loud to make sure you got them right. If anything seems off, call your pediatrician before giving the dose.
Are some families more at risk for medication errors?
Yes. Parents with limited health literacy are 2.3 times more likely to make dosing mistakes. Families with limited English proficiency have error rates as high as 45%, even when given translated instructions. Children on Medicaid are 27% more likely to experience medication errors due to fewer follow-up resources and less access to pharmacy counseling.
What’s being done to reduce these errors in hospitals?
Leading children’s hospitals use standardized weight-based dosing protocols, double-check systems for high-risk meds, and real-time pharmacy verification. Many now use electronic medical records with built-in pediatric dosing calculators. Some hospitals use pictograms and teach-back methods during discharge - reducing errors by up to 45%. Nationwide Children’s Hospital cut harmful events by 85% using these combined strategies.
Can technology help prevent these mistakes?
Yes. Pediatric-specific EMRs that auto-calculate doses based on weight reduce errors significantly. Dosing calculators built into hospital systems prevent manual math mistakes. Some apps let parents scan a prescription and get a visual dosing guide. But these tools are mostly in children’s hospitals - not general ERs. That’s a dangerous gap. Community hospitals need access to the same safety tech.
How much do these errors cost the healthcare system?
About 63,000 children visit emergency rooms each year because of home medication mistakes. That adds up to an estimated $28 million in emergency care costs annually. These are avoidable visits - caused by simple errors that could be prevented with better instructions, tools, and support.

 Health and Wellness
Health and Wellness
parth pandya
December 3, 2025 AT 09:49so many parents use kitchen spoons 😭 i work in a pediatric clinic and i’ve seen it a million times. even if they say ‘i know what a teaspoon is’-no you don’t. a tsp is 5mL, but most spoons are closer to 8-10mL. always use the syringe. always. i give them one with every script. simple fix, huge impact.
Joykrishna Banerjee
December 4, 2025 AT 11:10Let’s be frank: the real issue isn’t the syringe or the teach-back method-it’s the pathological infantilization of caregivers. We treat parents like toddlers who can’t handle basic pharmacokinetics. The solution isn’t pictograms, it’s education. Teach parents the *why* behind mg/kg dosing. Stop coddling. If you can’t calculate a dose based on weight, you shouldn’t be administering anything beyond aspirin. This isn’t a healthcare crisis-it’s a cognitive laziness epidemic.
Myson Jones
December 5, 2025 AT 03:17Thank you for writing this with such care. I’ve worked in ERs for 18 years, and I’ve seen too many families overwhelmed by instructions they don’t understand. The teach-back method isn’t just a protocol-it’s a lifeline. One mother told me, ‘I didn’t know the syringe wasn’t a spoon’-and she was crying because she thought she was a bad mom. We need to stop making people feel stupid for needing help. Simple tools, clear language, patience. That’s all it takes.
Albert Essel
December 6, 2025 AT 10:13There’s a profound irony here: we’ve engineered rockets to Mars, yet we still hand parents a plastic cup with ‘1 tsp’ printed on it and expect precision. The system isn’t broken-it’s archaic. We’ve digitized everything except the most human part: communication. Standardized dosing tools, pictograms, and EMR-integrated calculators aren’t luxuries. They’re ethical imperatives. If we can track a package across the globe, we can ensure a child gets the right dose.
Charles Moore
December 7, 2025 AT 17:23I’ve seen this in my own family. My niece’s mom gave her the wrong dose because the label said ‘for under 12kg’ and the kid was 13kg. She panicked, thought she’d killed her. We spent an hour on the phone with the pharmacist just to confirm it was safe. This shouldn’t be normal. The fact that we’re still relying on paper labels and verbal orders in 2024 is terrifying. I wish every pharmacy would include a QR code that links to a video demo of how to use the syringe. Simple. Free. Life-saving.
Gavin Boyne
December 7, 2025 AT 17:39Oh, so now we’re going to fix pediatric medication errors by giving parents *pictograms*? Brilliant. Next, we’ll hand them crayons to draw their own dosing schedules. Meanwhile, in the real world, 45% of non-English-speaking parents still mess up doses *even with translations*. We’re treating symptoms, not the disease: systemic neglect. The real fix? Hire bilingual pharmacists. Pay them. Give them time. Stop outsourcing safety to exhausted parents who are already juggling three jobs and a sick kid. The system’s not broken-it’s cruel.
Rashi Taliyan
December 8, 2025 AT 19:06I’m a mom of twins. One time I gave the wrong dose because I was up for 36 hours straight and my eyes were blurry. I didn’t realize I was reading the infant bottle instead of the children’s. I cried for an hour. I felt like a monster. But no one blamed me. The nurse just said, ‘Here, let me show you again.’ That’s the difference. Not blame. Not shame. Just patience. Please-don’t let anyone tell you it’s your fault. It’s the system’s fault. And thank you for saying that.
Kara Bysterbusch
December 10, 2025 AT 12:39There’s something quietly revolutionary about giving parents a syringe instead of a spoon. It’s not just about measurement-it’s about dignity. When you hand someone a tool designed for precision, you’re saying: ‘I trust you to handle this.’ That’s the missing ingredient. Not more instructions. Not more warnings. Just respect. And when you pair that with a photo of the label? You’re not just preventing error-you’re building confidence. And confidence, in a crisis, is everything.
Rashmin Patel
December 10, 2025 AT 14:30OMG I can’t believe this is still a thing in 2024 😭 I’m from India and we have the SAME PROBLEMS here-parents using tablespoons, pharmacists not labeling concentrations, doctors writing doses on sticky notes. My cousin’s baby got hospitalized because the nurse wrote ‘5mg’ but meant ‘5mL’ and the syrup was 120mg/5mL. The baby had seizures. It was avoidable. We need a national campaign-like ‘Don’t Use Spoons’-with Bollywood stars. Imagine Shah Rukh Khan saying ‘Use the Syringe, Not the Spoon!’ and then showing how. Viral. Memes. T-shirts. This isn’t just healthcare-it’s culture. And culture changes behavior. Let’s make safety cool.
sagar bhute
December 10, 2025 AT 23:13Let’s cut the fluff. This isn’t about ‘system failure.’ It’s about incompetence. Parents shouldn’t be administering medication at all. If you can’t read a label or do basic math, you shouldn’t be responsible for your child’s life. Stop blaming the system. Blame the people who can’t follow instructions. And stop pretending that pictograms fix ignorance. They don’t. They just make the hospital feel better about not training anyone. This is negligence dressed up as compassion.
Cindy Lopez
December 11, 2025 AT 16:4563,000 ER visits. $28 million. And we’re still using paper charts. This is embarrassing.
James Kerr
December 13, 2025 AT 12:55My kid had a fever last week. I used the syringe, double-checked the weight, took a pic of the label, and even texted my sister to confirm the dose. Felt like a NASA engineer. But honestly? It shouldn’t feel that hard. We’re making parents into pharmacists. Let’s fix the system so they don’t have to.
shalini vaishnav
December 14, 2025 AT 08:55Why do Western countries think they’re so advanced? In India, we’ve been using syringes for decades. We don’t need pictograms-we need discipline. Parents here are taught from day one: measure exactly, never guess. No spoons. No apps. Just responsibility. This whole ‘teach-back’ thing? It’s a sign of cultural weakness. We don’t need hand-holding. We need standards. And we need to stop outsourcing safety to technology.
Albert Essel
December 16, 2025 AT 06:16What’s fascinating is that the highest error rates aren’t in low-income areas-they’re in places where parents are overconfident. ‘I’m a doctor’s kid, I know what I’m doing.’ That’s when the worst mistakes happen. The ones who ask for help? They’re usually the safest.