
Medication Preferences Guide
Your Medication Preferences Guide
This tool helps you identify your preferences for medication decisions when you can't speak for yourself. Share these preferences with your healthcare proxy to ensure your wishes are respected.
How should pain be managed when you can't communicate your needs?
How would you like to handle antibiotics for infections when you have dementia or advanced illness?
What is your preference for blood thinners if you've had a history of falls or bleeding issues?
How should doctors manage confusion or agitation if you develop delirium?
How to use this guide
Share this summary with your healthcare proxy and your doctor. Print it and keep it with your medical power of attorney document. Update it annually or when your health situation changes.
Imagine you’re in the hospital after a stroke. You can’t speak. The doctors ask your family: Should we give her the blood thinner? What about the pain meds? Should we keep her on antibiotics? But no one knows what you’d want. That’s not a hypothetical. It happens every day. And it doesn’t have to.
What Is a Medical Power of Attorney?
A Medical Power of Attorney (also called a Healthcare Proxy or Durable Power of Attorney for Health Care) is a legal document that lets you pick someone you trust to make medical decisions for you if you ever can’t speak for yourself. It’s not about dying. It’s about making sure your voice still matters-even when you’re too sick to talk. This isn’t just for older people. Accidents happen. Strokes hit younger adults. Dementia creeps in slowly. You don’t need to be 80 to need this. You just need to be alive. The document only kicks in when your doctor says you’re no longer able to make or communicate your own choices. Until then, you’re still in charge. That’s the whole point: it’s a backup plan, not a surrender.Why Medication Decisions Are the Most Critical Part
Most people think advance directives are about life support-whether to hook you up to a ventilator or not. But in real hospitals, the biggest fights aren’t over machines. They’re over medications. A 2023 study in the Journal of Pain and Symptom Management found patients with a named healthcare agent had 32% fewer conflicts over medication choices during hospital stays. Why? Because doctors don’t just ask, “Do you want treatment?” They ask: “Should we give her this antibiotic? Should we stop the morphine? Can we give him the blood thinner, even if it might cause bleeding?” These aren’t easy calls. They’re messy. They’re emotional. They’re about quality of life, not just survival. Your agent needs to know:- Which pain meds you’re okay with-and which ones you refuse (like opioids, if you’ve had addiction issues)
- Whether you’d want antibiotics for an infection if you’re in late-stage dementia
- If you’d accept blood thinners even if you’ve had a fall before
- Whether you’d want medication to manage agitation if you develop delirium
How It’s Different From a Living Will
A living will says, “I don’t want to be on a machine if I’m brain dead.” That’s clear. But what if you get pneumonia? What if you’re confused and scared? What if you’re not dying-but you’re in pain and don’t want to be sedated? A living will can’t cover that. It’s a checklist. A Medical Power of Attorney is a person. Your agent can talk to doctors. They can ask questions. They can adapt. They can say, “She always said she didn’t want to be in pain, even if it meant she’d be awake.” Or, “He always said he’d take any pill to stay out of the nursing home.” The Mayo Clinic says it best: “A living will doesn’t cover every situation.” That’s why you need both-but if you can only do one, pick the agent.Who Should Be Your Agent?
Not your spouse. Not your oldest child. Not the one who says they’ll “handle it.” Pick the person who:- Knows your values-not just your medical history
- Can say “no” to doctors when they push for more treatment
- Won’t be pressured by other family members
- Has actually talked to you about what matters to you

What the Form Actually Lets Them Do
The legal document gives your agent the right to:- Decide whether you get a new medication-or stop one
- Choose between oral pills or IV injections
- Refuse treatments that don’t match your wishes
- Access your medical records
- Talk to doctors, nurses, and social workers on your behalf
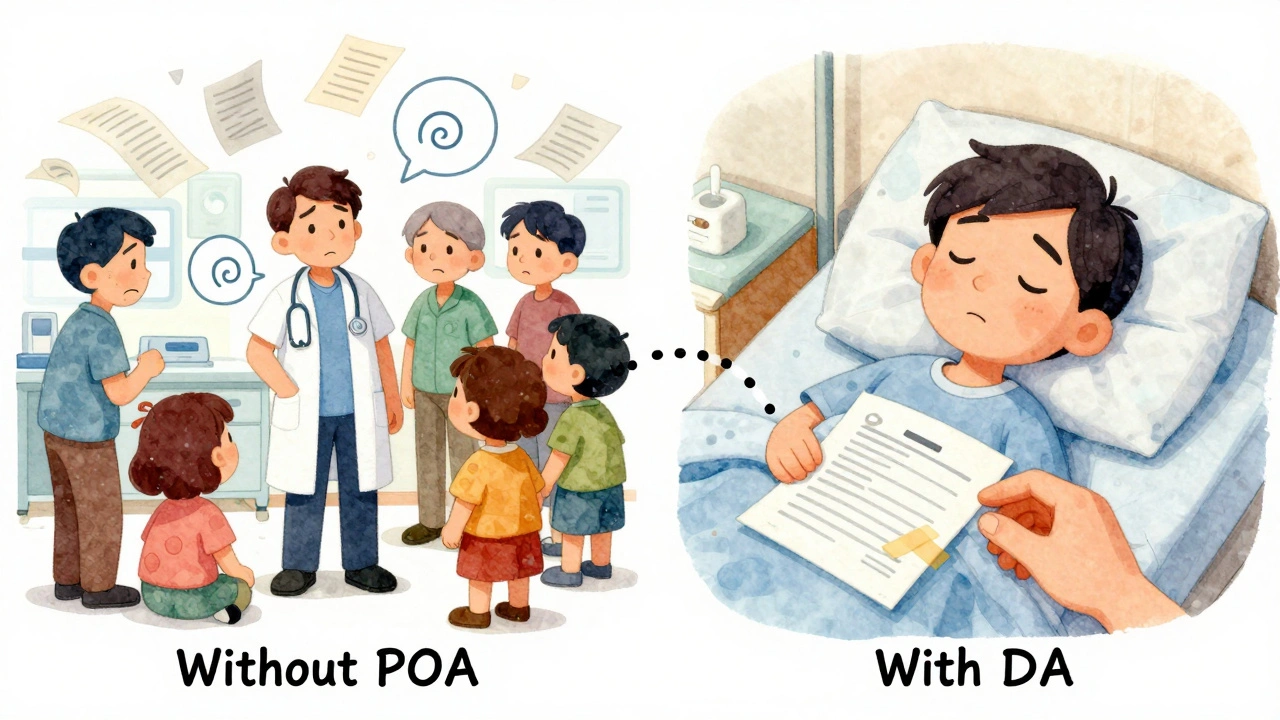
What Happens If You Don’t Have One?
Without a Medical Power of Attorney, the law steps in. Usually, it’s your spouse, then adult children, then parents. But what if you’re divorced? What if your kids don’t get along? What if your mom thinks you’d want everything done-and your brother thinks you’d want peace? That’s when hospitals call ethics committees. That’s when delays happen. That’s when you get a feeding tube you never wanted-or you’re kept on painkillers that make you groggy for weeks. One Reddit user, NurseJen42, shared how her mother’s POA prevented a 12-hour delay in antibiotics during sepsis. The hospital couldn’t give the drug without consent. The agent was there. The agent knew her mom hated IVs and wanted oral meds first. They gave the right dose, on time. She went home. Another family spent three days arguing over whether to give an antipsychotic to their father with dementia. No one knew what he’d said. No one had talked about it. He ended up sedated for a week.How to Get Started (Step by Step)
You don’t need a lawyer. You don’t need to pay $500. Here’s how to do it in under an hour:- Choose your agent. Talk to them first. Make sure they say yes.
- Download your state’s form. Go to LawHelp DC or your state’s health website. Most are free.
- Fill it out. Sign it. Get witnesses or notarize it (check your state’s rules).
- Have the conversation. Sit down with your agent. Go through every medication scenario you can think of. Write down your answers.
- Give copies to everyone. Your agent, your doctor, your pharmacist, your family. Keep one in your wallet.
- Review it yearly. If you get a new diagnosis, change your mind, or your agent moves away-update it.
Common Mistakes (And How to Avoid Them)
- Mistake: Thinking the form is enough. Fix: Talk. Talk again. Talk until it’s uncomfortable.
- Mistake: Picking someone because they’re “responsible.” Fix: Pick someone who knows your soul, not just your schedule.
- Mistake: Not telling your doctor. Fix: Give them a copy. Ask them to put it in your chart.
- Mistake: Waiting until you’re sick. Fix: Do it now. Today. While you can still think clearly.
What About POLST or MOLST?
If you’re seriously ill-say, advanced cancer, heart failure, or late-stage dementia-you might also need a POLST (Physician Orders for Life-Sustaining Treatment). This isn’t a substitute for a Medical Power of Attorney. It’s a companion. POLST is a medical order. It’s signed by your doctor. It says: “Do not resuscitate,” “No IV fluids,” “No antibiotics.” It goes in your chart. It’s honored in 47 states. But it doesn’t replace your agent. It just gives clear instructions for specific situations. If your condition changes, your agent can still update things. POLST is for when you’re close to the end. Your Medical Power of Attorney is for everything else.You’re Not Giving Up Control. You’re Taking Back Power.
This isn’t about death. It’s about dignity. It’s about not being a burden. It’s about making sure the last thing your body feels isn’t confusion-but peace. You don’t have to be old. You don’t have to be sick. You just have to care enough to speak up now-so your voice isn’t lost later. Start today. Talk to one person. Fill out one form. Write down one thing you’d never want. Your future self will thank you.Can a Medical Power of Attorney override my doctor’s advice?
No. Your agent can’t force a doctor to give you a treatment that goes against medical standards or hospital policy. But they can refuse treatments you don’t want-even if the doctor recommends them. The agent’s job is to honor your wishes, not to override medical judgment.
Do I need a lawyer to create a Medical Power of Attorney?
No. Every state offers free, legally valid forms online through health departments or legal aid sites like LawHelp DC. You just need to sign it in front of witnesses or a notary-depending on your state’s rules. A lawyer is only needed if your situation is complex, like having multiple marriages, blended families, or mental health conditions.
Can my agent make decisions about psychiatric medications?
In most states, yes-but not always. Some states, like Indiana, require a doctor to certify you’re incapacitated before your agent can decide on psychiatric drugs. Others allow it without extra steps. Check your state’s rules. The key is to discuss your feelings about these meds with your agent ahead of time-whether you’d accept them for severe anxiety, refuse them due to past side effects, or only want them in emergencies.
What if my family disagrees with my agent’s decisions?
If your agent has a legally valid Medical Power of Attorney, their decisions stand-even if family members object. Hospitals follow the law, not popular opinion. That’s why choosing the right person is so important. If you’re worried about conflict, talk to your family ahead of time. Say, “I’ve chosen [Name] because they know me best. I trust them to make the right call.”
How often should I update my Medical Power of Attorney?
Review it at least once a year-and anytime you have a major life change: a new diagnosis, a divorce, a death in the family, or if your agent moves away or becomes unable to serve. Your values might change too. What you wanted at 50 might not be what you want at 70. Update it as often as your health changes.

 Health and Wellness
Health and Wellness
Victoria Graci
December 3, 2025 AT 08:24It’s wild how we’ll plan for every damn thing-life insurance, pet trusts, even what Spotify playlist plays at our funeral-but still act like death is a surprise party we can RSVP to later. This isn’t about dying. It’s about refusing to let the system turn your body into a bureaucratic puzzle. I keep a laminated card in my wallet with my meds I refuse, my agent’s number, and one line: ‘She’d rather be quiet than drugged.’ That’s it. No lawyer needed. Just clarity.
And yeah, the ‘blood thinner’ thing? My aunt didn’t know they weren’t for ‘thinning blood’ like maple syrup. She thought they were dangerous because her ex-husband called them ‘poison.’ Turns out, they kept her from a second stroke. We didn’t talk about it until it was too late. Don’t be her.
Saravanan Sathyanandha
December 5, 2025 AT 05:47In India, we often assume family will ‘know’ what’s right. But when my uncle was in ICU after a cardiac arrest, his sister insisted on full code-despite him having whispered to me three years prior, ‘If I’m breathing with a machine, I’m already gone.’ No paperwork. No conversation. Just guilt and tears and a feeding tube he never wanted.
Medical POA isn’t Western. It’s human. It’s saying: ‘I trust you enough to carry my voice when I can’t speak.’ It’s not about law. It’s about love that’s brave enough to be specific.
Fern Marder
December 5, 2025 AT 09:49OMG YES. 🙌 I just did this last week after my mom’s ER visit. I told my brother, ‘If I’m drooling and staring at the ceiling like a confused pigeon, don’t let them give me morphine. I hate how it makes me feel like a zombie.’ He cried. Then he said, ‘Why didn’t you tell me this before?’
So now I have a Google Doc titled ‘My Dying Rules (No Jokes).’ It’s got bullet points, memes, and a photo of me at 23 holding a margarita. If I can’t talk, they’ve got proof I’d rather be buzzed than sedated. 😎
Zoe Bray
December 7, 2025 AT 00:57While the emotional appeal of this article is compelling, it is critically important to emphasize the legal and institutional frameworks that govern healthcare decision-making. The Medical Power of Attorney (MPOA) is a subset of advance care planning under the Patient Self-Determination Act (PSDA) of 1990, which mandates that healthcare institutions inform patients of their rights to execute advance directives.
However, the efficacy of MPOA is contingent upon interprofessional coordination, electronic health record (EHR) integration, and clinician awareness. Studies indicate that only 42% of MPOA documents are accessible at the point of care due to fragmentation in documentation systems. Therefore, while the moral imperative is clear, systemic implementation remains the primary barrier to patient autonomy.
Recommendation: Integrate MPOA documentation into EHR templates with automated alerts for clinicians during triage. Without structural reform, individual agency remains insufficient.
Girish Padia
December 7, 2025 AT 02:22People act like this is some big secret. Nah. It’s just lazy. You don’t wanna talk about death? Fine. But don’t cry when your kid’s stuck deciding if Mom gets antibiotics or not. You think hospitals care? They don’t. They just want to move beds.
I saw a guy in the ER last month. His daughter had no idea if he wanted pain meds. He was 62. Had diabetes. Wasn’t old. Just didn’t talk. Now he’s got a feeding tube and his wife’s in therapy. Don’t be that guy. Do the thing. Now.
william tao
December 7, 2025 AT 04:17Another feel-good article from the wellness-industrial complex. You’re telling me the solution to America’s broken healthcare system is... a piece of paper? And a ‘conversation’? That’s it?
Meanwhile, 12 million Americans can’t afford insulin. Hospitals are turning away Medicaid patients. And you want me to believe that if I just tell my sister I hate morphine, everything will be fine?
It’s not about ‘dignity.’ It’s about a system that treats human life like a cost center. Fix that. Not your Google Doc.
Sandi Allen
December 8, 2025 AT 22:26John Biesecker
December 9, 2025 AT 08:51bro i just did this last night. i sat with my mom and we went through every med i’ve ever taken. i told her if i ever get dementia and start screaming at the wall, don’t give me the antipsychotic unless i’m hurting someone. she said ‘what if you’re just scared?’ and i said ‘then hold my hand.’ we cried. then we ordered pizza.
i saved the doc on my phone under ‘my dying instructions (dont laugh)’ and sent it to her, my dr, and my dog walker. yeah, my dog walker. she’s the only one who knows i hate hospitals.
also, i put a sticky note on my fridge: ‘if i’m not laughing, don’t feed me.’ it’s dumb. but it’s mine.
Kristen Yates
December 9, 2025 AT 12:52