CGM Trend Arrow Dose Adjustment Calculator
How to Use This Tool
Enter your current glucose level, trend arrow, correction factor, and patient type to calculate the proper insulin adjustment. This tool follows Endocrine Society guidelines for safe dose adjustments.
When you're managing diabetes with insulin or other medications, the biggest fear isn't just high blood sugar-it's the sudden, dangerous drop that comes out of nowhere. A CGM doesn't just show you your number right now. It tells you where it's headed. And that changes everything.
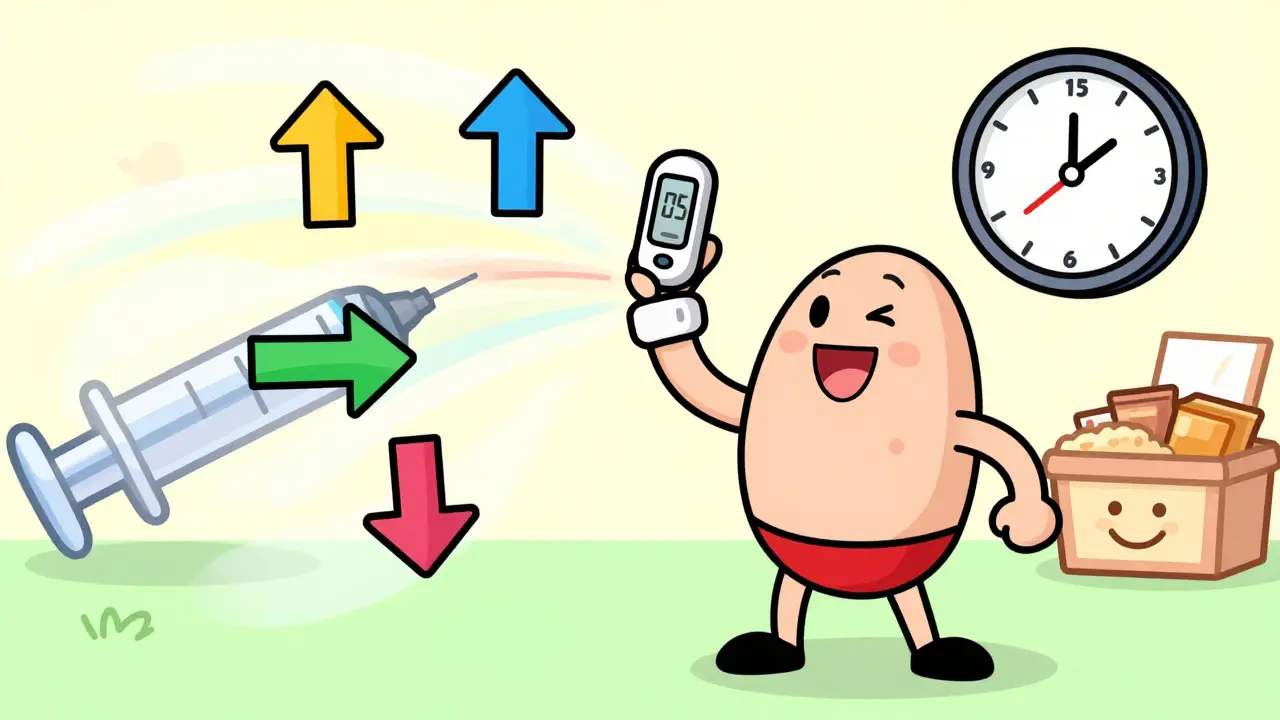
Why Trend Arrows Matter More Than Your Last Glucose Reading
A blood sugar meter gives you a snapshot. A CGM gives you a movie. The trend arrows-up, down, flat, double-up, double-down-are your early warning system. They show you if your glucose is racing toward a low or climbing fast toward a high, often 15 to 30 minutes before it hits the danger zone. This isn’t guesswork. It’s science. In 2017, the Endocrine Society published clear guidelines on how to use these arrows to adjust insulin doses. Their research showed people who used trend arrows cut their hypoglycemic events by 28% and spent 17% more time in target range compared to those relying only on fingersticks. The key is acting before the number gets bad. If your glucose is rising fast before breakfast, you can add a little extra insulin now to prevent a spike. If it’s falling quickly at 2 a.m., you can reduce your nighttime basal or eat a small snack before it crashes. That’s the power of predictive dosing.How to Read Your CGM Trend Arrows (And What to Do)
Most CGMs, like Dexcom G5, G6, and G7, use the same five trend arrows:- Double-up (↑↑): Glucose rising faster than 2 mg/dL per minute
- Single-up (↑): Glucose rising between 1 and 2 mg/dL per minute
- Flat (→): Glucose stable, changing less than 1 mg/dL per minute
- Single-down (↓): Glucose falling between 1 and 2 mg/dL per minute
- Double-down (↓↓): Glucose falling faster than 2 mg/dL per minute
- Double-up arrow: Add 1.2 units to your pre-meal or correction dose
- Single-up arrow: Add 0.8 units
- Flat arrow: No change
- Single-down arrow: Reduce dose by 0.8 units
- Double-down arrow: Reduce dose by 1.2 units
Don’t Just Follow the Arrow-Know Your Insulin Timing
Here’s where people get tripped up. Trend arrows tell you where glucose is going, but they don’t tell you what’s already in your body. If you took insulin 45 minutes ago and your glucose is now falling fast, adding more insulin will make it worse. That’s called insulin stacking-and it’s one of the leading causes of severe lows in new CGM users. Always ask: How much insulin is still active? Rapid-acting insulins like Humalog, NovoLog, or Fiasp peak around 60-90 minutes after injection and last 4-5 hours. If you took a bolus recently, subtract the remaining active insulin from your new dose. A simple rule: If you’re unsure, wait. Check your glucose again in 15 minutes. If the arrow is still pointing down and you’re below target, eat 15 grams of fast-acting carbs-not a full meal. Then recheck in 15.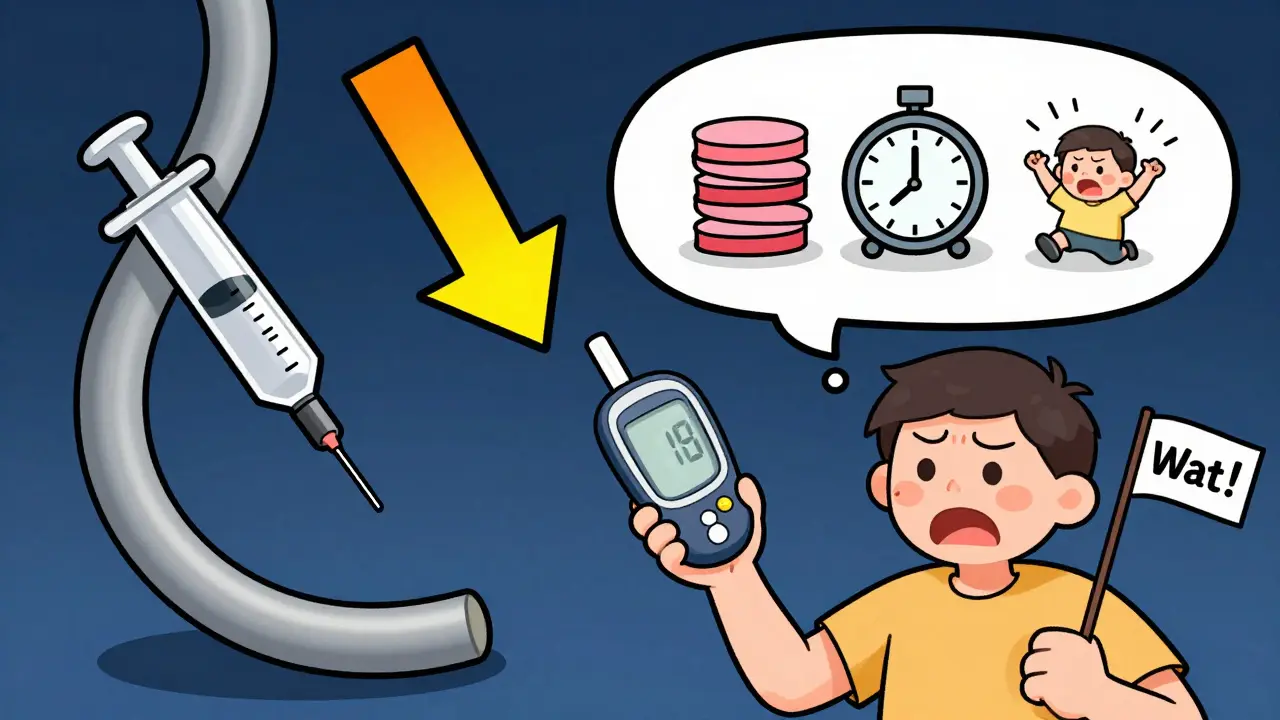
What About Non-Insulin Medications?
Most people think CGM adjustments only apply to insulin. But newer guidelines from the ADA and EASD in 2024 now recommend adjusting non-insulin drugs too. For example, SGLT2 inhibitors like Jardiance or Farxiga work by making your kidneys flush out sugar. But if your glucose is consistently low or trending down-especially with ketones above 0.6 mmol/L-you’re at risk for euglycemic diabetic ketoacidosis (euDKA), a rare but dangerous condition. If your CGM shows:- Glucose under 180 mg/dL
- And ketones above 0.6 mmol/L
- And a consistent downward trend
Common Mistakes and How to Avoid Them
People jump into CGM dose adjustments with excitement-and then make the same errors over and over. Mistake 1: Adjusting during sensor warm-up or after signal loss. CGM readings can lag or be inaccurate for up to 2 hours after sensor start-up or after you’ve been sweating, showering, or moving a lot. Wait until the sensor is stable and the trend arrow is consistent for at least 15 minutes before adjusting. Mistake 2: Ignoring your correction factor. Your insulin sensitivity isn’t the same as your friend’s. If you’re 1:30 (1 unit lowers glucose by 30 mg/dL), you need smaller adjustments than someone who’s 1:70. Know your number. Test it by taking a correction dose and checking glucose every 30 minutes for 2 hours. Mistake 3: Overcorrecting for double-down arrows. If your glucose is dropping fast, your instinct is to eat something. But if you’re on insulin and just ate, eating more can cause a rebound spike. Instead, reduce your next insulin dose by the recommended amount, and wait. If you’re below 70 mg/dL, treat with 15g carbs, not 30. Mistake 4: Not talking to your provider. A 2023 JAMA study found only 31% of primary care doctors feel confident teaching CGM dose adjustments. Don’t assume your provider knows this. Bring the Endocrine Society guidelines. Ask for a 20-minute education session. Print out the adjustment tables. Most CGM companies offer free printable guides-use them.
Real Results: What People Are Actually Doing
On Reddit’s r/typeonegrit, one user named InsulinWizard42 reduced their weekly lows from 3.2 to 0.7 after using the Endocrine Society method. They said: “The unit-based adjustments took the guesswork out of dosing. I didn’t have to calculate percentages-I just added or subtracted what the table said.” But not everyone gets it right. A user on Diabetes Daily doubled their insulin for a double-up arrow without checking their insulin-on-board and ended up with a 45 mg/dL low. That’s why education matters. A 2021 survey by Beyond Type 1 found that 68% of CGM users adjust doses using trend arrows. Of those, 82% saw better time-in-range. The other 32% didn’t use them-mostly because they were scared of messing up or hadn’t been taught how.What’s Next? AI, Apps, and the Future of Dosing
The next leap isn’t just arrows-it’s automation. In 2023, the FDA cleared the first app-DAFNE+-that automatically calculates your dose adjustment based on your CGM data and insulin settings. In trials, it cut user error by 62%. Companies like Verily are using machine learning to predict glucose trends beyond what the arrows show. One pilot study showed 38% fewer lows by anticipating drops 45 minutes ahead. But technology won’t replace understanding. Even the smartest app can’t know if you’re sick, stressed, or just had a long walk. You still need to know your body. You still need to know your insulin. You still need to know when to trust the arrow-and when to pause.Getting Started: Your 3-Step Plan
If you’re new to CGM dose adjustments, here’s how to begin safely:- Know your correction factor. Test it by taking a correction dose and checking glucose every 30 minutes for 2 hours. Write it down.
- Learn the arrow adjustments. Print the Endocrine Society tables. Tape them to your fridge or phone case. Use them for a week without changing anything else.
- Ask for help. Schedule a 20-minute visit with your diabetes educator or endocrinologist. Show them your CGM data. Ask: “Am I adjusting correctly?”
Can I adjust my diabetes medication dose based on CGM trend arrows if I’m not on insulin?
Yes-but only under medical supervision. While insulin users follow clear dose adjustment tables, non-insulin medications like SGLT2 inhibitors (Jardiance, Farxiga) may need dose reduction if CGM shows persistent low glucose combined with ketones above 0.6 mmol/L. This prevents a rare but dangerous condition called euglycemic diabetic ketoacidosis. Always consult your provider before changing any medication dose.
How often should I check my insulin correction factor?
Test your correction factor every 3 to 6 months, or sooner if you’ve gained or lost weight, started new medications, or noticed more frequent highs or lows. Your sensitivity can change due to stress, illness, or aging. The best way to test it: take a correction dose when your glucose is above target, then check every 30 minutes for 2 hours to see how much it drops. Average the results over 3 tests for accuracy.
What if my CGM shows a double-down arrow but I feel fine?
CGMs can sometimes lag or give false readings, especially during rapid changes or after physical activity. If you feel fine but your CGM shows a fast drop, confirm with a fingerstick test. If your meter matches the CGM and your glucose is below 80 mg/dL, reduce your next insulin dose by the recommended amount. If you’re above 80 mg/dL and feel okay, wait 15 minutes and check again. Don’t treat a trend-you treat a number that’s confirmed and falling.
Are all CGMs the same when it comes to trend arrows?
No. Dexcom uses double arrows for glucose changes faster than 2 mg/dL per minute. Abbott’s FreeStyle Libre uses them for changes faster than 3 mg/dL per minute. That means the same arrow on two different devices doesn’t mean the same thing. Always check your device’s manual for how it defines each arrow. The Endocrine Society guidelines were built for Dexcom data, but the principles apply to all CGMs-you just need to adjust the speed thresholds based on your device’s specs.
Can I use trend arrows to adjust my basal insulin?
Not directly. Trend arrows are meant for bolus (mealtime and correction) insulin adjustments. Basal insulin is for background control and should be adjusted based on overnight or fasting glucose patterns over several days, not single trends. If you see consistent low or high trends overnight for 3+ nights, that’s when you talk to your provider about adjusting your basal rate. Using arrows for basal changes can lead to dangerous stacking or unstable glucose.

 Health and Wellness
Health and Wellness
Nicholas Miter
January 25, 2026 AT 01:24Been using trend arrows for about 6 months now. Honestly, the biggest shift wasn't the numbers-it was the peace of mind. No more panic at 3 a.m. wondering if I'm gonna crash. If the arrow's pointing down, I just chill and wait 15 minutes. Most times it levels out. If not, I grab a glucose tab. Simple.
Also learned the hard way not to trust arrows during workouts. Sensor lag is real. Always double-check with a fingerstick after sweating.
Biggest win? My A1c dropped from 7.8 to 6.9. No magic, just consistency.
Suresh Kumar Govindan
January 25, 2026 AT 07:02It is imperative to note that the Endocrine Society guidelines are not universally applicable. Their data cohort was predominantly Caucasian, insulin-dependent adults, with negligible representation from South Asian populations, who exhibit markedly different insulin kinetics. To apply these dosing protocols without calibration to ethnic metabolic variance constitutes a form of medical colonialism.
TONY ADAMS
January 25, 2026 AT 15:43bro i tried this and went from 150 to 42 in 20 mins. i was like ‘ok i got this’ and added more insulin because the arrow was up?? what the hell. now i’m scared to even look at my cgms. thanks for nothing.
Josh josh
January 25, 2026 AT 20:54man i just use the arrows like a compass not a gps
if its down i dont dose
if its up i dose a lil
if its flat i eat
if its double down i eat and wait
no math no stress
my sugar stays in range
thats all i need
Rakesh Kakkad
January 26, 2026 AT 05:34While the utility of trend arrows is undeniably beneficial, one must exercise caution regarding the temporal latency inherent in continuous glucose monitoring systems. The physiological lag between interstitial fluid glucose and venous blood glucose may result in misinterpretation of dynamic trends, particularly during postprandial states or acute exercise. Therefore, algorithmic adjustments must be tempered with clinical judgment and corroborated by capillary blood glucose measurements.
Betty Bomber
January 28, 2026 AT 01:43Just wanted to say this post saved me. I used to treat every single drop like a crisis. Now I wait. I breathe. I check my fingerstick. Most of the time, I’m fine. The arrows are a warning, not a panic button.
Also, I print the tables and stick them on my fridge. It’s weirdly comforting.
Mohammed Rizvi
January 29, 2026 AT 03:52Oh so now we’re giving CGMs a personality? ‘The arrow is sad’ ‘The arrow is mad’ ‘The arrow is plotting my demise’
Look, if you’re gonna use these tools, use them right. Don’t turn your glucose monitor into a fortune teller. Know your correction factor. Know your insulin timing. Or else you’ll be the guy who crashes at 2 a.m. because he thought ‘double down’ meant ‘eat a whole pizza’.
eric fert
January 29, 2026 AT 13:02Let’s be real-this whole trend-arrow thing is just a fancy way of saying ‘guess more accurately.’ The Endocrine Society guidelines? Written by people who’ve never had to wake up at 3 a.m. to give their kid juice while their own glucose is dropping. And don’t get me started on the ‘kids’ adjustments. You’re telling me a 12-year-old’s insulin sensitivity is predictable enough to apply a fixed 0.6-unit reduction? That’s not science, that’s wishful thinking.
Also, the JAMA study says only 31% of doctors know how to teach this? Then why are we treating this like gospel? Because it’s easy? Because it sounds smart? Because it makes us feel in control?
Here’s the truth: glucose is chaos. No algorithm, no arrow, no table can tame it. You think you’re mastering your diabetes? You’re just dancing with it. And sometimes, the dance ends with you on the floor.
Ashley Karanja
January 31, 2026 AT 08:42There’s a profound epistemological shift here-from reactive glycemic management to anticipatory physiological modulation. The CGM trend arrow, as a proximal indicator of interstitial glucose kinetics, functions not merely as a diagnostic tool but as a phenomenological interface between metabolic autonomy and algorithmic guidance. The integration of dynamic insulin dosing based on temporal slope vectors represents a paradigmatic evolution in self-regulatory diabetes care, transcending the Cartesian binary of ‘high’ and ‘low’ into a continuous, probabilistic field of metabolic potentiality.
However, the ontological reliability of this interface remains contingent upon sensor fidelity, pharmacokinetic individuality, and the absence of confounding variables such as cortisol spikes, dehydration, or circadian phase shifts. Thus, while the data-driven adjustment protocol is statistically validated, its phenomenological efficacy remains deeply embodied and contextually emergent-not reducible to a table, but experienced as a dialogue between body and machine.
Karen Droege
January 31, 2026 AT 08:56THIS. IS. LIFE-CHANGING. I used to have 5 lows a week. Now? Zero. I printed the table. I taped it to my insulin pen. I even made a sticky note on my phone lock screen. I used to think I was being ‘careful’ by overcorrecting. Turns out, I was just being reckless.
Also, I told my mom about this. She’s 68 and on metformin. She doesn’t use insulin, but now she checks her glucose before yoga because she saw the part about SGLT2 inhibitors and euDKA. She’s not diabetic, but she’s learning. That’s the power of this post.
Thank you. Seriously. You didn’t just give me a tip-you gave me my life back.
bella nash
February 2, 2026 AT 04:01The utilization of trend arrows as a determinant of insulin dosage modification presupposes a homogeneity of physiological response that is neither empirically substantiated nor theoretically tenable. The reduction of metabolic regulation to a binary schema of directional vectors obfuscates the multivariate nature of glycemic homeostasis, wherein hormonal flux, circadian rhythm, and psychosocial stressors interact in nonlinear fashion. Consequently, the prescriptive application of fixed unit adjustments constitutes a form of medical reductionism that may, paradoxically, increase the incidence of iatrogenic hypoglycemia.
Geoff Miskinis
February 4, 2026 AT 02:30It’s amusing how people treat these arrows like divine revelation. The Dexcom guidelines were written for a specific population under controlled conditions. Real-world usage? People are eating candy bars, drinking alcohol, and sleeping with their sensors under pillows. You can’t apply a 1.2-unit adjustment to someone who had three beers and a burrito. This isn’t medicine-it’s a cult.
And why do we assume the ‘double-down’ means ‘reduce insulin’? What if it’s because your basal is too high? Or you’re sick? Or you’re in ketosis? No one ever talks about the context. Just follow the arrow. Like a robot.
Sally Dalton
February 4, 2026 AT 02:31i just wanted to say thank you for writing this. i’ve been scared to touch my insulin since i got my cgm. i thought i’d mess up and crash. but reading this made me feel like i could actually learn this. i printed the table and i’m gonna try it this week. no pressure, just baby steps. you’re right-it’s about preventing lows, not just reacting to them.
also, i have a typo on my phone but i don’t care anymore. i’m just glad i’m not alone.
Shawn Raja
February 4, 2026 AT 22:11Let’s be honest-this whole system is just a glorified game of ‘guess the trend.’
I’ve had my CGM for two years. I’ve had more lows since I started using arrows than before. Why? Because I trusted the machine over my body. I felt fine. My glucose was 85. Arrow said ‘double-down.’ So I reduced my insulin. Next thing I know, I’m at 58. I didn’t need to adjust-I needed to eat. But I listened to the arrow instead of my gut.
And now I’m paranoid. Every time I feel a little shaky, I check my CGM. And if the arrow moves, I panic. So I eat. Then I spike. Then I dose. Then I crash. It’s a loop.
Maybe the real problem isn’t the arrows. Maybe it’s that we’ve outsourced our intuition to a gadget.
Still… I’m gonna keep using it. Because I’m scared to stop.