
When your pupils shrink down to tiny dots under bright light, that’s myosis. It’s not a disease-it’s a normal reaction. But when it happens without reason, or stays stuck that way, it can throw off an eye exam and lead to wrong diagnoses. Many patients walk out of an eye clinic confused because their vision feels fine, yet the doctor says something’s wrong. Often, the real issue isn’t their eyes-it’s how myosis messed with the test.
What Myosis Really Is
Myosis means your pupils are smaller than they should be. Normal pupils range from 2 to 8 millimeters wide, depending on light. In bright rooms, they shrink. In the dark, they open up. That’s how your eyes protect the retina and adjust vision. Myosis happens when pupils stay too small-even in low light. This isn’t just about light sensitivity. It’s a signal your nervous system is sending something off.
It’s not rare. Up to 15% of people over 60 show signs of persistent myosis without obvious cause. It can come from medications like glaucoma drops, opioids, or even some antidepressants. It can also be caused by nerve damage, head injuries, or conditions like Horner’s syndrome. In some cases, it’s the first clue that something deeper is going on.
Why Myosis Skews Eye Exams
Eye doctors rely on seeing the back of your eye-the retina, optic nerve, blood vessels. To do that, they dilate your pupils with drops. But if your pupils are already too small from myosis, those drops might not work. The dilation takes longer, or doesn’t happen at all. That means the doctor can’t see the full picture.
Imagine trying to look through a keyhole. You might catch a glimpse, but you’ll miss the corners. Same with an eye exam. If the pupil won’t open, the doctor can’t spot early signs of diabetic retinopathy, macular degeneration, or glaucoma. These conditions start with tiny changes. Miss those, and you miss the window to stop damage.
Some clinics use special imaging tools like OCT scans. But even those need a clear view. If the pupil is constricted, the image gets blurry or incomplete. That leads to repeat visits, wasted time, and unnecessary anxiety for the patient.
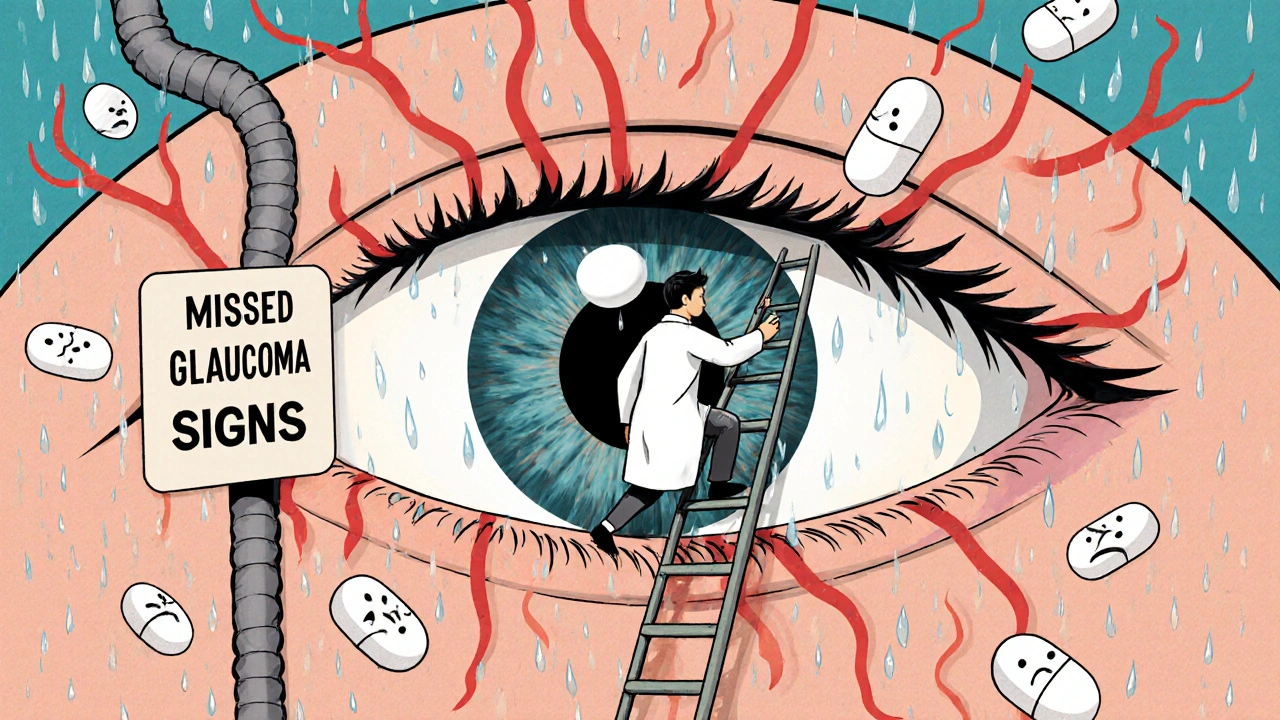
How Myosis Masks Glaucoma
Glaucoma is called the silent thief of sight because it often shows no symptoms until it’s advanced. One of the main tests is measuring intraocular pressure. But pressure readings can be falsely low if the pupil is constricted. Why? Because the shape of the eye changes slightly when the iris is pulled tight. That changes how fluid flows inside, making pressure seem normal when it’s actually high.
Doctors also check the optic nerve for damage. A small pupil hides the edge of the nerve head. That’s where early glaucoma shows up-as a slight cupping or thinning. If you can’t see it clearly, you might think everything’s fine. Then, years later, the patient loses peripheral vision. And it was all missed because the pupil stayed too small.
One 2023 study in the Journal of Ophthalmology found that 22% of patients with undiagnosed glaucoma had undetected myosis during their last exam. In half of those cases, the doctor didn’t even note the pupil size in the chart.
Medications That Cause Myosis
Many common drugs cause pupils to shrink. People don’t realize this affects their eye health. Here’s what to watch for:
- Pilocarpine-used for glaucoma. It’s meant to lower pressure, but it also shrinks pupils permanently in some users.
- Opioids-morphine, oxycodone, heroin. These trigger the parasympathetic nervous system, which controls pupil size.
- Cholinesterase inhibitors-used for Alzheimer’s and myasthenia gravis. They increase acetylcholine, which tightens the iris.
- Clonidine-a blood pressure drug. Can cause chronic myosis in up to 18% of long-term users.
- SSRIs-some antidepressants like fluoxetine and sertraline. Less common, but documented.
If you’re on any of these and your pupils are always small, tell your eye doctor. Bring your medication list. It’s not just about side effects-it’s about accurate diagnosis.
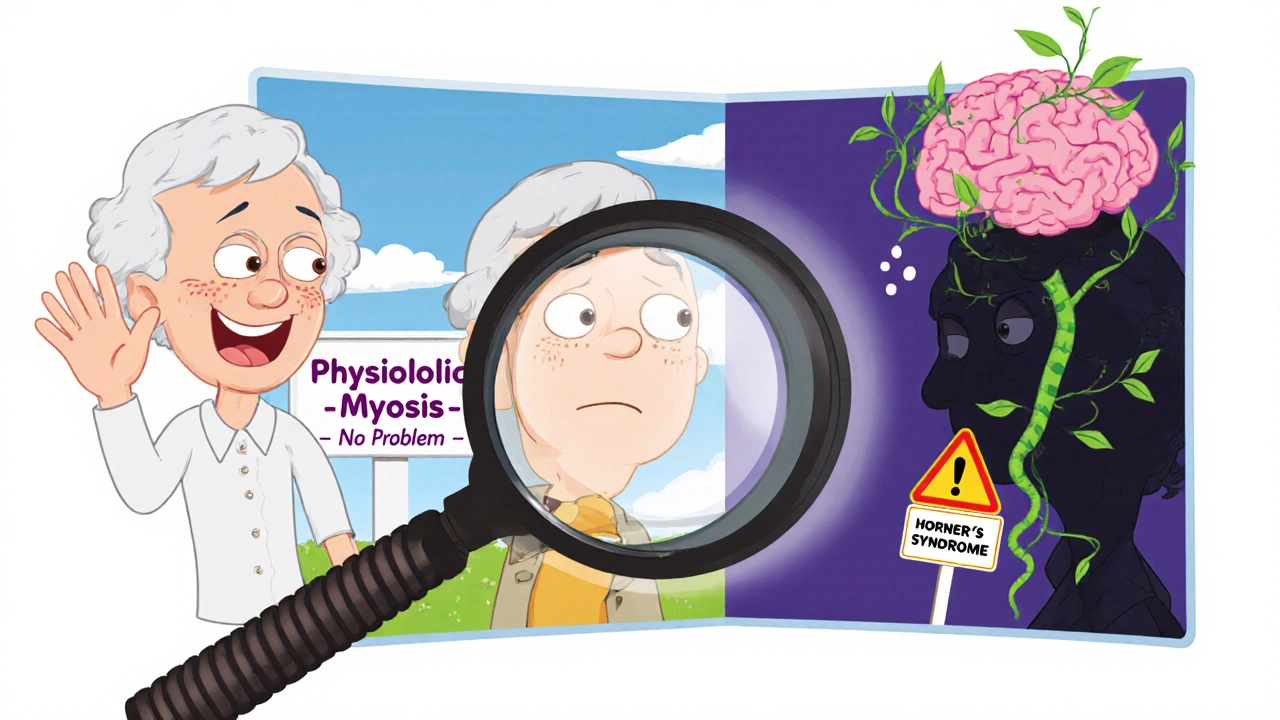
Myosis as a Clue to Neurological Problems
Not all myosis is harmless. If one pupil is smaller than the other, and doesn’t react to light, that’s a red flag. It could mean Horner’s syndrome-a condition caused by damage to the sympathetic nerve pathway. This can come from a neck injury, tumor, or even a stroke.
Doctors check for this with a simple test: they use apraclonidine drops. If the small pupil gets bigger after the drop, it confirms Horner’s. That’s important because the underlying cause could be life-threatening. A tumor in the lung, for example, can press on the nerve and cause one-sided myosis long before any cough or pain shows up.
Even in older adults, sudden myosis without obvious cause should raise questions. A 2024 study in Neurology Today showed that 1 in 12 patients with unexplained myosis had an undiagnosed brainstem lesion. These patients were misdiagnosed with age-related vision loss-until a neurologist noticed the pupil mismatch.
What Patients Can Do
You don’t need to be a doctor to help get an accurate eye exam. Here’s what works:
- Before your appointment, note if your pupils are always small-even in dim rooms.
- Write down every medication you take, including supplements and over-the-counter drugs.
- If you’ve had eye surgery, head trauma, or nerve issues, mention it.
- Ask: “Can you see the full retina? If not, why?”
- If dilation fails, ask if they can use a different imaging method, like wide-field photography.
Don’t assume the doctor knows. Many don’t check pupil size unless it looks abnormal. But myosis isn’t always obvious. It’s subtle. And it’s often ignored.
What Eye Doctors Should Do
Good eye care starts with measuring pupils-not just guessing. Every exam should include:
- Recording pupil size in millimeters in both light and dark.
- Testing reaction to light and near focus.
- Comparing both pupils for symmetry.
- Noting any medications that could cause myosis.
- Using pupilometers if available-they give exact measurements, not estimates.
If dilation fails, don’t just say “we’ll try again.” Try alternative tools. Some clinics now use handheld OCT devices that work with smaller pupils. Others use blue-light imaging to enhance contrast. These aren’t luxuries-they’re necessary when myosis is present.
Also, document everything. If a patient has persistent myosis, flag it in their chart. It’s not just a footnote. It’s a diagnostic variable.
When Myosis Isn’t a Problem
Not every small pupil means trouble. Some people naturally have small pupils. It’s called physiologic myosis. It’s harmless and runs in families. If both pupils are equal, react normally, and the person has no symptoms, no action is needed.
The key is consistency. If your pupils have always been small since you were young, and your vision hasn’t changed, it’s likely normal. But if they suddenly got smaller, or one changed more than the other-that’s when you need to dig deeper.
Final Thought: Don’t Let a Tiny Pupil Hide a Big Problem
Myosis is easy to overlook. It doesn’t hurt. It doesn’t blur vision. It doesn’t make you squint. But it can hide glaucoma, stroke, tumors, and nerve damage. A pupil that’s too small is like a locked door. The doctor can’t see what’s behind it.
Patients, speak up. Doctors, measure it. It’s not about being paranoid. It’s about making sure nothing slips through the cracks. Your eyes don’t lie. But sometimes, the tools we use to look at them do-if we don’t account for myosis.

 Health and Wellness
Health and Wellness
Jonathan Gabriel
November 20, 2025 AT 02:56So let me get this straight-your pupils are like a stubborn door that won’t open, and suddenly your retina’s got a VIP pass to nowhere? 😅
My grandma’s on glaucoma drops and her pupils look like two black BBs. She thought she was ‘seeing better’ until her optometrist finally asked, ‘Why are you squinting in the dark?’
Turns out, she’d been getting false negatives for years. This post? Gold. Someone should turn this into a pamphlet and hand it out with every prescription.
Don Angel
November 20, 2025 AT 06:48Wow. Just… wow. I didn’t realize how many meds could do this. I’m on clonidine for blood pressure, and I’ve always thought my ‘sensitive eyes’ were just aging. But now I’m wondering-did my last eye exam miss something? I’ll bring my med list next time. Seriously, this changed my perspective.
Also, can we please make pupil measurement mandatory? Like, a checkbox on every form? It’s not hard. It’s just… overlooked.
deepak kumar
November 21, 2025 AT 22:54As someone from India where eye care access is still a luxury for many, this is critical. In rural clinics, doctors often skip pupil checks entirely-they’re rushing through 50 patients a day. I’ve seen people get misdiagnosed with ‘presbyopia’ when it was actually myosis masking glaucoma.
But here’s the thing: even in cities, patients don’t speak up. They trust the doctor. That’s cultural. We need awareness campaigns in local languages. Maybe a short video in Hindi or Tamil? I’d help make one.
Dave Pritchard
November 21, 2025 AT 23:05Thank you for writing this. I’m a nurse who works with elderly patients, and I’ve seen this exact scenario too many times. One lady came in saying she ‘couldn’t see the clock’-but her vision was fine. Her pupils were pinpricks from SSRIs. The doctor blamed her ‘old age.’
She came back six months later with vision loss. We finally caught it. This isn’t just medical-it’s human. Please share this with your doctor. Seriously.
And if you’re on meds that shrink pupils? Don’t be shy. Bring a list. It’s not annoying. It’s lifesaving.
kim pu
November 22, 2025 AT 15:31Okay but… what if the whole eye exam industry is just a $12 billion scam built on pretending they can see your retina? What if myosis is just the tip of the iceberg? What if they’ve been using outdated tech because they don’t want to admit they’re blind to the real problem?
Also, did you know the FDA approved pupil-dilating drops that were tested on 12 people? Twelve. I’m not paranoid. I’m… informed.
And why is no one talking about the fact that 80% of eye clinics still use flashlights to measure pupils? It’s 2025. We have phones with LiDAR. Use it.
malik recoba
November 23, 2025 AT 04:56i never thought about this before but wow. my dad had glaucoma and they missed it for years. he thought he was just getting old. now i’m gonna check his meds and ask his doc about pupil size. thanks for this. it’s simple but important. i’ll tell my aunt too. she’s on those alzheimer’s pills. maybe she needs a new eye dr.
Sarbjit Singh
November 24, 2025 AT 04:06This is so important!! 😊 I’m a retired optician in Delhi and I’ve seen this over and over. One time, a man came in with ‘blurry vision’-turns out his pupils were tiny from opioid painkillers after a back injury. We didn’t dilate him because we thought he was ‘just nervous.’ He lost 30% of his vision before we figured it out.
Always ask. Always check. Always write it down. 🙏
Angela J
November 24, 2025 AT 17:20Wait… so you’re saying the eye doctors don’t even check pupil size? And the pharmaceutical companies know this? And they’re not telling you? And the FDA is asleep? And this is why so many people go blind? This isn’t negligence-it’s a cover-up. I’ve been saying this for years.
They don’t want you to know that your glaucoma meds might be hiding your real diagnosis. It’s all connected. The drops, the cameras, the ‘normal’ readings-they’re all part of the system.
Bring a mirror to your next appointment. Look at your pupils. Then ask: ‘Why are you hiding this from me?’
Sameer Tawde
November 25, 2025 AT 18:30Simple fix: measure pupils. Every. Single. Time.
It takes 5 seconds. Costs nothing. Could save a lifetime.
Doctors: stop guessing. Start measuring.
Patients: speak up. Bring your meds.
Done.
Erica Lundy
November 27, 2025 AT 13:49The epistemological implications of myosis as a diagnostic occlusion are profound. The phenomenological experience of vision is mediated not merely by photoreceptor function, but by the ontological constraints of pupillary aperture-a liminal space where biological regulation intersects with epistemic limitation.
One must therefore question: if the instrument of observation is itself constrained by pharmacological or neurological interference, can the observed phenomenon ever be considered ‘true’? Or is diagnosis merely an artifact of instrumental inadequacy?
Perhaps the retina does not lie-but the apparatus through which we perceive it does.
Kevin Jones
November 28, 2025 AT 08:36MYOSIS IS THE SILENT KILLER OF VISION. NOT GLAUCOMA. NOT DIABETES. NOT MACULAR DEGENERATION.
IT’S THE FACT THAT NO ONE CHECKS THE PUPILS.
THEY’RE LOOKING AT THE RETINA THROUGH A KEYHOLE AND CALLING IT A DIAGNOSIS.
WE’RE IN A POST-MEDICAL ERA WHERE TECHNOLOGY IS SUPPOSED TO HELP-BUT WE’RE STILL USING FLASHLIGHTS AND GUESSWORK.
THIS ISN’T MEDICINE. IT’S A CRIME.
STOP IGNORING THE PUPILS.
Premanka Goswami
November 29, 2025 AT 05:39Okay, but what if myosis isn’t natural at all? What if it’s caused by 5G radiation? Or the microchips in vaccines? Or the new smart streetlights that emit ‘pupil-constricting frequencies’? I’ve noticed my pupils have been smaller since the city installed those LED bulbs last year.
And why is everyone ignoring the fact that the WHO doesn’t even list myosis as a ‘public health concern’? Coincidence? I think not.
They don’t want you to know that your eyes are being manipulated. But I do. And now you do too.
Bring a UV light to your next appointment. Test your pupils. Ask them: ‘Why won’t you answer?’