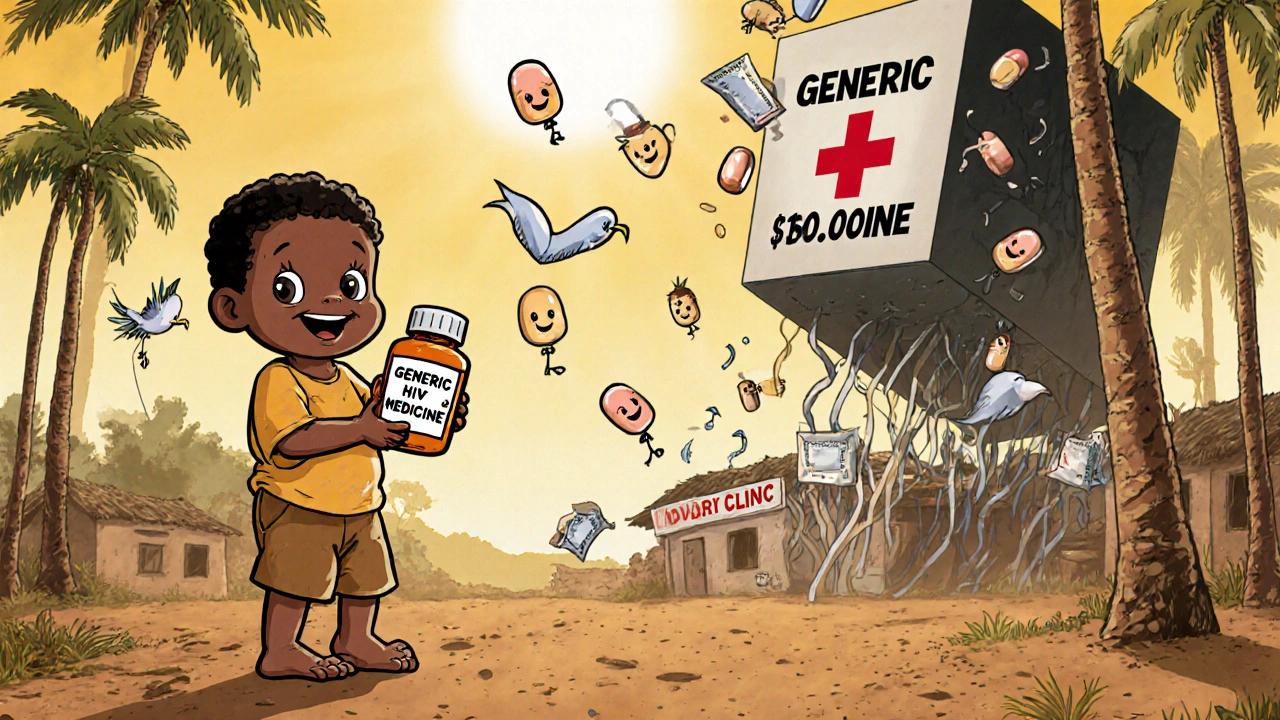
Two billion people around the world can’t get the medicines they need. Not because the drugs don’t exist, but because they’re too expensive. In low-income countries, a single course of antibiotics, HIV treatment, or insulin can cost more than a week’s wages. The solution isn’t magic. It’s not new technology. It’s generics.
What Are Generics, Really?
Generics are exact copies of brand-name drugs. Same active ingredient. Same dosage. Same way they work in your body. The only difference? No patent. No marketing. No fancy packaging. That’s why they cost 80% less. In the U.S., 9 out of 10 prescriptions are filled with generics. In low-income countries? Only 1 in 20. Why? It’s not because people don’t want them. It’s because the system is broken. The World Health Organization says safe, affordable medicines are a human right. Yet, in places like rural Nigeria, Bangladesh, or rural Peru, getting a generic drug isn’t just about money-it’s about access, trust, and infrastructure.Why Generics Should Be Everywhere-But Aren’t
Take HIV treatment. In the early 2000s, branded antiretrovirals cost over $10,000 a year per person. Generic versions dropped that to under $100. Millions of lives were saved. That’s not theory. That’s fact. In sub-Saharan Africa, generic drugs turned HIV from a death sentence into a manageable condition. But that success story didn’t spread evenly. Why? First, many countries still have high import taxes and tariffs on medicines. A drug that costs $5 to make might end up costing $20 by the time it reaches a clinic because of red tape and fees. Second, regulatory systems are slow. In some places, it takes years to approve a generic drug-even when it’s already approved in the U.S. or Europe. Meanwhile, people die waiting. Third, there’s fear. Patients and even doctors worry generics are fake or weak. That’s not always true. Many generic manufacturers in India, South Africa, and Brazil meet international quality standards. But without clear labeling or public trust campaigns, people stick with expensive brands-even if they can’t afford them.The Real Cost of Not Using Generics
It’s not just about health. It’s about poverty. Nearly 90% of people in low-income countries pay for medicine out of their own pockets. No insurance. No safety net. When a family spends half their income on a single drug, they skip meals. Pull kids out of school. Sell livestock. That’s how illness pushes people into extreme poverty. The World Bank says 100 million people are pushed into extreme poverty every year because of healthcare costs. That’s not a statistic. That’s a mother choosing between her child’s medicine and food. That’s a farmer skipping treatment for malaria because he can’t afford it-and loses his harvest. Generics could stop this. But only if they’re available, trusted, and priced right.
Who’s Making Generics-and Who’s Not Helping
Five big generic companies-Cipla, Hikma, Sun Pharma, Teva, and Viatris-make 90% of the off-patent drugs that low-income countries need. But a 2024 analysis found they only had clear plans to make 41 of those drugs affordable for the poorest patients. Most strategies ignored the reality: people can’t buy medicine if they’re living on $2 a day. Big pharma companies like Pfizer and Novartis have programs to help. They offer discounts or donate drugs. But they rarely say how many people actually get them. Transparency is missing. Without knowing who’s being helped, we can’t fix what’s broken. Meanwhile, countries like India and South Africa have built strong generic manufacturing industries. But they’re still blocked by trade rules, patent extensions, and lack of investment in local distribution.What’s Working-And Where
Some places are getting it right. In Thailand, the government negotiated bulk prices for HIV generics and set up public clinics to distribute them. Today, over 90% of HIV patients get treatment. In Rwanda, the government partnered with NGOs and local pharmacies to deliver generics directly to villages. Tuberculosis treatment rates jumped. In Ghana, a program called the Essential Drugs Program cut drug prices by 70% by eliminating middlemen and taxing imports at zero. More people got medicine. More kids survived. The pattern? When governments take charge-cutting taxes, speeding up approvals, and investing in supply chains-generics work.The Missing Pieces: Supply Chains, Trust, and Policy
It’s not enough to make cheap drugs. You have to get them to people. In many rural areas, there’s no reliable power for refrigerators. No roads. No pharmacies. A drug that survives the journey from India might spoil before it reaches a clinic. And then there’s the trust gap. People see fake drugs on the market. They hear stories. So they pay more for the brand-even if it’s the same pill in a different box. Solutions? Simple, but hard to implement:- Remove import taxes and tariffs on essential medicines.
- Speed up drug approval with WHO pre-qualification as a shortcut.
- Train community health workers to explain generics and fight misinformation.
- Use QR codes or tamper-proof labels to verify real generics.
- Invest in cold chain logistics for medicines that need refrigeration.


 Health and Wellness
Health and Wellness
Scott McKenzie
November 28, 2025 AT 11:19Just saw this and had to say - generics saved my dad’s life in rural India. He was paying $300/month for brand-name insulin. Found a WHO-approved generic for $8. Same pill. Same results. He’s alive today because someone didn’t let corporate greed win. 🙌
Jeremy Mattocks
November 30, 2025 AT 05:46Let me break this down real simple. The reason generics aren’t everywhere isn’t because they don’t work - it’s because the system is rigged. Big pharma spends billions lobbying to extend patents, block parallel imports, and scare patients with fear campaigns about ‘unsafe generics.’ Meanwhile, people in Bangladesh are choosing between feeding their kids and buying a $50 vial of fake antibiotics that look like the real thing. We’ve got the tech to verify real generics with QR codes. We’ve got factories in India making quality drugs. We’ve got the WHO pre-qualification system. What we don’t have is political will. And until governments stop treating medicine like a luxury good and start treating it like a public utility, nothing changes. It’s not rocket science. It’s just ethics.
Paul Baker
November 30, 2025 AT 18:58Jill Ann Hays
December 2, 2025 AT 06:40Mike Rothschild
December 3, 2025 AT 21:29Ron Prince
December 4, 2025 AT 22:52King Splinter
December 6, 2025 AT 11:46Kristy Sanchez
December 7, 2025 AT 06:48Michael Friend
December 7, 2025 AT 13:53They always do this. They show you the success stories - Rwanda, Thailand - and pretend it’s easy. But what about the 90% of countries where the government is corrupt, the roads are dirt, and the pharmacists are illiterate? You think a QR code helps when people can’t read? You think a WHO stamp means anything when the local clinic sells expired meds to make rent? This isn’t a policy problem. It’s a human problem. And humans are messy. And broken. And we can’t fix them with a spreadsheet.
Jerrod Davis
December 9, 2025 AT 01:38Dominic Fuchs
December 9, 2025 AT 20:27Asbury (Ash) Taylor
December 11, 2025 AT 10:00Kenneth Lewis
December 12, 2025 AT 22:22Jim Daly
December 14, 2025 AT 16:04Tionne Myles-Smith
December 15, 2025 AT 02:59Okay but let’s talk about the real heroes - the community health workers in Ghana who walk 10 miles with a cooler full of insulin to reach a village. No pay. No recognition. Just pure grit. They’re the ones keeping people alive while CEOs count their bonuses. We need to celebrate them, not just the drugs. And maybe, just maybe, if we start listening to the people on the ground instead of the people in boardrooms, we’ll actually fix this.