
Fentanyl Patch Heat Exposure Calculator
Heat Exposure Risk Assessment
Calculate how heat exposure affects fentanyl absorption. Based on FDA warnings: temperatures above 37°C (98.6°F) can increase absorption by 25-50%.
Results will appear here after calculation
Important Safety Note
This calculator estimates absorption increases based on article data. NEVER adjust patch dosage based on this tool. Always follow your doctor's instructions and seek immediate medical help for overdose symptoms.
When a doctor prescribes a Fentanyl patch is a transdermal opioid delivery system designed for continuous, long‑term pain relief, most patients focus on the pain relief and forget the hidden dangers lurking beneath the sticky coating. The reality is that these patches can turn a daily dose into a life‑threatening emergency if they’re not used exactly as instructed. Below we break down the most common side effects, the warning signs of overdose, and what happens when the patch is removed too quickly.
Why the Fentanyl Patch Is Different From Other Opioids
The patch delivers fentanyl straight through the skin for up to 72 hours, maintaining a steady blood level without the peaks and troughs of oral pills. That steady stream is great for chronic cancer or severe non‑cancer pain, but it also means the drug stays in the system for days after removal. A small increase in skin temperature-fever, a hot bath, or even a heating pad-can boost absorption by 25‑50 % and push a therapeutic dose into the toxic range.
Common Side Effects You’ll See Early On
- Dry mouth and constipation
- Drowsiness or “brain fog”
- Nausea or mild vomiting
- Reduced appetite
- Sweating, especially at night
These effects are usually mild when the dose matches the patient’s opioid tolerance. If you notice anything more severe-like sudden confusion, severe dizziness, or a rapid heartbeat-you’re likely stepping into the overdose zone.
Recognizing an Overdose Early
Because the patch releases a constant dose, overdose symptoms often develop slowly, giving a false sense of security. Watch for these red flags:
| Symptom | Overdose | Withdrawal |
|---|---|---|
| Breathing | Slow, shallow, or stopped | Rapid, shallow |
| Consciousness | Extreme drowsiness, inability to wake | Restlessness, agitation |
| Pupil size | Pinpoint (very small) | Dilated (large) |
| Skin | Cold, clammy, bluish lips | Sweaty, flushed |
| Heart rate | Very slow or irregular | Elevated, palpitations |
| Other | Seizures, loss of coordination | Yawning, teary eyes, nausea |
If any overdose signs appear, remove the patch immediately, call emergency services (911 in the US, 000 in Australia), and administer naloxone if it’s available.
Understanding Withdrawal: Why Stopping Cold Is Dangerous
Fentanyl creates physical dependence quickly. When the patch is taken off or the dose is cut too sharply, the body reacts with a cascade of withdrawal symptoms that can be both uncomfortable and medically risky. According to the U.S. Food and Drug Administration (FDA), abrupt discontinuation has been linked to severe pain spikes, dehydration, and even suicidal thoughts.
Typical withdrawal timeline:
- 8‑24 hours after last dose - early signs (yawning, sweating, anxiety)
- 36‑72 hours - peak intensity (muscle aches, nausea, vomiting, rapid heart rate)
- 7‑10 days - most symptoms subside, but cravings and mood swings may linger for weeks
Because the fentanyl patch maintains a baseline concentration for days, a sudden stop can leave the brain starving for opioid activity, prompting the nervous system to go into overdrive.
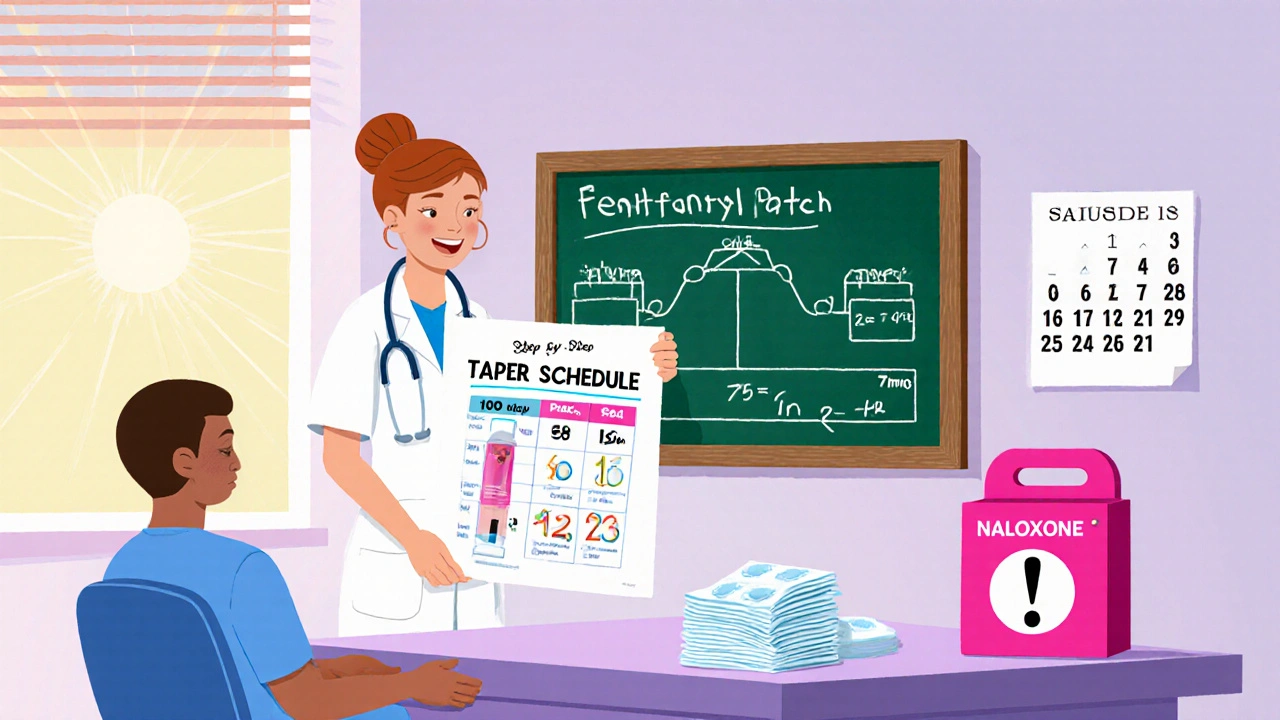
Safe Tapering Strategies Recommended by Experts
The American Society of Addiction Medicine (ASAM) advises reducing the patch dose by no more than 10‑25 % every 1‑3 weeks, depending on the starting strength. A typical taper might look like this for a patient on a 100 mcg/hour patch:
- Week 1‑2: Switch to 75 mcg/hour
- Week 3‑4: Switch to 50 mcg/hour
- Week 5‑6: Switch to 25 mcg/hour
- Week 7‑8: Switch to 12 mcg/hour or discontinue with a rescue plan
During tapering, clinicians monitor pain scores, withdrawal checklists, and any signs of relapse. Patients should keep a daily log of symptoms and report any sudden spikes in pain or mood changes.
Key Risk‑Mitigation Measures (REMS) You Should Know
Since 2012, the Risk Evaluation and Mitigation Strategy (REMS) has required doctors and pharmacies to provide counseling on safe use, storage, and disposal. Important points:
- Store patches in a sealed container out of reach of children-32 accidental pediatric deaths were recorded between 1997‑2012.
- Never apply a new patch to the same skin site within 24 hours; rotate sites to avoid irritation.
- Avoid heat sources (heating pads, hot tubs, sunny windowsills) while the patch is on.
- Dispose of used patches by folding the sticky sides together and placing them in a puncture‑proof container.
- Ask your prescriber for a rescue kit that includes naloxone and instructions on how to use it.
Special Populations: Children, the Elderly, and Opioid‑Naïve Patients
Children are especially vulnerable because their skin absorbs fentanyl more quickly. Even a single used patch can cause fatal respiratory depression. For elderly patients with thin skin, the risk of higher absorption increases, and they often have comorbidities that magnify respiratory depression.
The patch is contraindicated for opioid‑naïve individuals. If a clinician tries to start therapy in someone without an established opioid tolerance (generally defined as at least 60 mg morphine‑equivalent per day for a week), the chance of overdose jumps dramatically.
When to Call Your Doctor vs. Emergency Services
Call your doctor if you notice any of the following:
- Persistent nausea or vomiting lasting more than 24 hours
- New or worsening skin irritation at the application site
- Increasing drowsiness that interferes with daily activities
- Signs of mild withdrawal while the patch is still in place (e.g., yawning, sweating)
Call emergency services immediately for any breathing difficulties, unresponsiveness, or signs of overdose listed earlier.
Bottom Line: Stay Informed, Stay Safe
The fentanyl patch is a powerful tool when used correctly, but its potency makes it a double‑edged sword. Understanding the side‑effect profile, recognizing overdose and withdrawal signs, and following a clinician‑guided taper can keep you out of the hospital-and keep your pain under control.
Can I wear two fentanyl patches at once to increase pain relief?
No. Adding a second patch raises the dose dramatically and can cause fatal respiratory depression. Always follow the prescribed dose and talk to your doctor before any change.
What should I do if the patch falls off accidentally?
If the adhesive side is still intact, re‑apply it to a clean, dry area of intact skin. If the patch is damaged or the adhesive is compromised, discard it safely and contact your prescriber for a replacement.
Is it safe to take a hot shower while wearing a fentanyl patch?
A warm shower is okay, but avoid hot tubs, saunas, or heating pads. High temperatures can increase skin absorption by up to half, pushing you toward an overdose.
How long does it take for withdrawal symptoms to appear after I stop using the patch?
Symptoms usually start within 8‑24 hours, peak between 36‑72 hours, and may last a week or more. A gradual taper reduces both intensity and duration.
Should I keep a naloxone kit at home if I’m on a fentanyl patch?
Yes. The FDA now recommends that anyone prescribed a fentanyl patch receive a naloxone prescription or have easy access to an over‑the‑counter kit.

 Health and Wellness
Health and Wellness
Kathryn Rude
October 24, 2025 AT 14:05The pharmacokinetics of a fentanyl patch are not just a medical detail, they are a moral mirror reflecting our shortcut culture 😊
When you slap a drug that seeps through skin you are betting on a constant whisper of death, not a steady comfort.
The patch's silent delivery challenges the illusion of control we cling to in modern pain management.
Ignoring the temperature‑induced absorption spike is akin to flirting with a loaded gun while claiming you only want to feel warm.
So before you praise the convenience, contemplate the invisible gamble you are taking.
Marilyn Pientka
November 6, 2025 AT 04:33From an ethical pharmacovigilance standpoint, the indiscriminate endorsement of transdermal fentanyl violates the principle of non‑maleficence, a cornerstone of biomedical ontology.
The posited benefits are obfuscated by a cavalier neglect of thermodynamic absorption variables, thereby contravening established dosing algorithms.
Such cavalier discourse erodes the fiduciary trust between prescriber and patient, precipitating a cascade of iatrogenic morbidity.
It is incumbent upon responsible clinicians to promulgate stringent adherence to REMS protocols, lest we succumb to systemic complacency.
Jordan Levine
November 18, 2025 AT 22:06Yo, the patch is like a ticking time bomb strapped to your skin, and you think it's just for pain? 🇺🇸💥
If you can't handle the heat, stop messing with the big leagues of opioids!
This is not a game, it's life or death, and nobody's gonna save you if you ignore the warning signs! 🚨🔥
Mary Mundane
December 1, 2025 AT 15:40Your glorification of the patch ignores the stark realities of overdose risk.
Dahmir Dennis
December 14, 2025 AT 09:13Ah, the fentanyl patch – the darling of modern analgesia, hailed as a panacea for chronic sufferers while simultaneously masquerading as a silent assassin.
One would think that such a marvel of pharmaceutical engineering would come with a user manual written in plain English, but no, we are instead handed a litany of legalese that would make a contract lawyer weep.
The notion that a small adhesive square can maintain a constant plasma concentration without any peaks is as romantic as it is dangerously naive.
Yet, the literature is replete with case reports where a casual hot shower transformed a therapeutic dose into a fatal overdose, a fact that seems to escape the glossy brochures.
Perhaps the most egregious oversight is the assumption that patients will not experiment with heat sources, as if every individual lacks the curiosity of a cat.
When the patch is removed abruptly, the withdrawal cascade can rival the intensity of a severe flu, complete with nausea, vomiting, and an existential dread that no physician can easily allay.
The recommended tapering schedule-10 to 25 percent reductions every one to three weeks-reads like a culinary recipe, demanding patience and precise measurement that most of us simply do not possess.
Moreover, the REMS program, while well‑intentioned, often feels like an administrative maze designed to obfuscate rather than protect the patient.
One must also consider the pediatric danger; a single used patch can be lethal to a child, a grim reality that is too easily glossed over in outpatient settings.
The irony is palpable: a device meant to alleviate suffering becomes a conduit for potential catastrophe if mishandled.
Healthcare providers, in their ivory‑tower wisdom, sometimes neglect to emphasize the simple yet crucial advice: avoid heat, rotate sites, and keep naloxone handy.
Patients, on the other hand, may feel a false sense of security, believing that the patch’s steady delivery eliminates the need for vigilance.
This complacency is a breeding ground for tragedy, as demonstrated by countless emergency department visits stemming from misguided confidence.
In truth, the fentanyl patch is a double‑edged sword, demanding both reverence and restraint from all parties involved.
So before you slap another patch onto your skin, pause and reflect on the cascade of physiological fireworks you might be igniting.
And remember, the best safety net is an informed patient who respects the potency of the drug rather than treating it as a mere convenience.
Jacqueline Galvan
December 27, 2025 AT 02:46Thank you for the thorough overview; I’d like to add a few practical points that may help patients navigate the taper safely.
First, maintain a daily diary noting pain scores, any skin irritation, and mood changes – this data can guide dose adjustments.
Second, coordinate with your prescriber to have a rescue plan that includes a low‑dose breakthrough medication for breakthrough pain spikes during tapering.
Third, keep a naloxone kit within reach and ensure a trusted family member knows how to administer it.
Finally, avoid any external heat sources, even a hot yoga class, as even modest temperature rises can increase fentanyl absorption significantly.
Following these steps can reduce the risk of both overdose and severe withdrawal while preserving quality of life.
Dawn Bengel
January 8, 2026 AT 20:20The United States has poured billions into the opioid crisis, yet we keep handing out these patches like candy 🍬🔥.
If you think a “tiny” patch can’t hurt you, think again – it’s a potent opioid that can silence an entire nation’s breathing if misused.
Take responsibility: store them out of children’s reach, never heat them up, and for God’s sake, have naloxone on hand! 💪🇺🇸
Our health system will crumble if we keep treating this as a minor inconvenience.
Dason Avery
January 21, 2026 AT 13:53Consider the patch not merely as a medication but as a partnership with your body – a delicate balance between relief and risk.
When you honor that balance, you honor yourself, and the journey becomes less about control and more about coexistence.
Every time you rotate sites, you’re writing a small act of self‑respect into your daily routine.
Stay vigilant, stay informed, and remember that the greatest power lies in knowledge, not in the dosage you wear on your skin. 🌟
HILDA GONZALEZ SARAVIA
February 3, 2026 AT 07:26I’ve been wondering about the exact timeline for withdrawal after discontinuing a high‑dose fentanyl patch.
From the literature, symptoms can begin as early as eight hours, peak around thirty‑six to seventy‑two hours, and linger for several days, but individual variability is huge.
Do clinicians typically schedule follow‑up visits during that window, or is it left to patient‑initiated contact?
Any insight into how to best monitor and report these symptoms would be greatly appreciated.