
DRESS Syndrome Diagnostic Calculator
Assess DRESS Risk
The RegiSCAR scoring system evaluates 5 clinical criteria to determine likelihood of Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS). This tool helps identify cases that require immediate medical attention.
Symptom Assessment
Laboratory Criteria
DRESS syndrome isn’t just a rash. It’s a full-body crisis triggered by a medication you likely thought was safe. Imagine taking a pill for gout, epilepsy, or an infection, and weeks later, your skin breaks out in a fiery red rash, your fever spikes above 38.5°C, your lymph nodes swell, and your liver starts failing. That’s DRESS - Drug Reaction with Eosinophilia and Systemic Symptoms. It doesn’t come on fast like a flu. It creeps up, often after 2 to 8 weeks, which is why it’s so often missed. By the time doctors realize what’s happening, organs are already damaged. And in about 1 in 10 cases, it’s fatal.
How DRESS Starts - And Why It’s So Easy to Miss
DRESS doesn’t begin with a single symptom. It starts quietly. A low-grade fever. A few red spots on your chest. Maybe your throat feels a little sore. You think it’s a virus. You take more ibuprofen. You wait it out. But under the surface, your immune system is going haywire. The drug you took - maybe allopurinol, carbamazepine, or vancomycin - has triggered a deadly chain reaction. Your body starts producing too many eosinophils, a type of white blood cell meant to fight parasites. Instead, they attack your own tissues. Liver enzymes climb. Kidneys struggle. Lungs fill with fluid. And the rash? It spreads across 80-90% of your body.
What makes DRESS so sneaky is the delay. Most drug rashes show up within days. DRESS waits. That’s why emergency rooms see the same patient three or four times before anyone connects the dots. One patient on Reddit described visiting the ER three times over five weeks. Each time, she was told it was allergies or a viral infection. Only when her ALT liver enzyme hit 1,200 IU/L - nearly 40 times the normal level - did a dermatologist say: "This is DRESS. Stop everything. Now."
Who’s at Risk? The Real Culprits Behind DRESS
Not every drug causes DRESS. But some are notorious. Allopurinol, used for gout, accounts for nearly 30% of cases. Anticonvulsants like carbamazepine and phenytoin make up another quarter. Antibiotics like vancomycin and sulfonamides are also common triggers. Even some antivirals and NSAIDs have been linked. But here’s the twist: not everyone who takes these drugs gets DRESS. Genetics play a huge role.
If you carry the HLA-B*58:01 gene variant, your risk of allopurinol-induced DRESS jumps dramatically. That’s why Taiwan started screening everyone before prescribing allopurinol - and cut DRESS cases by 80%. In the U.S., that screening isn’t routine. People with HLA-A*31:01 are at higher risk with carbamazepine. These aren’t rare mutations. They’re common in certain populations. Yet most doctors don’t test for them.
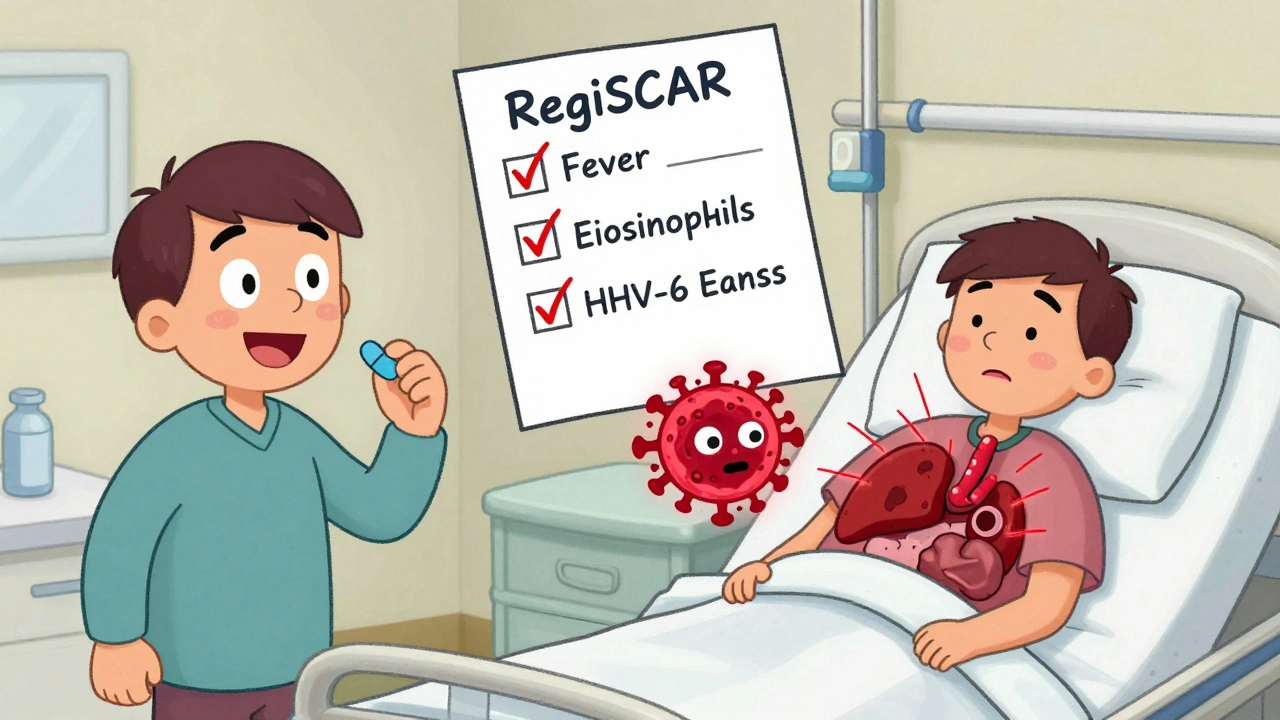
And it’s not just the drug. Viral reactivation is part of the puzzle. In 60-80% of DRESS cases, HHV-6 - a virus most people carry silently - wakes up and starts replicating. That’s not a coincidence. It’s a trigger. The drug messes with your immune control, the virus reawakens, and your body goes into overdrive. That’s why antiviral drugs are sometimes used alongside steroids.
The Diagnostic Puzzle - RegiSCAR Is Your Best Tool
There’s no single blood test for DRESS. Diagnosis is a checklist. The RegiSCAR scoring system is the gold standard. It looks at five things: timing of the rash after starting the drug, fever, enlarged lymph nodes, blood abnormalities (especially eosinophils over 1,500), and organ involvement. Each point adds up. A score of 4 or higher means probable DRESS. 5 or more? Definite.
Doctors who use RegiSCAR get it right 97% of the time. But most don’t. A 2021 study found only 38% of primary care doctors could correctly identify DRESS criteria. That’s why so many patients are misdiagnosed. A rash with fever? Easy to call it measles. Liver enzymes up? Must be hepatitis. Eosinophils high? Allergies. But DRESS is a system failure - not a single organ. You need to see the whole picture.
Key labs to check: CBC with differential (look for eosinophilia), liver enzymes (ALT, AST), creatinine, and viral serologies for HHV-6, EBV, CMV. A skin biopsy can help, but it’s not always needed. The pattern of organ involvement - liver first, then kidneys, then lungs - is more telling than any single test.
What Happens If You Don’t Act Fast
Delay kills. The longer DRESS goes untreated, the worse the damage. Liver failure. Kidney shutdown. Heart inflammation. Pulmonary infiltrates. Some patients develop chronic autoimmune diseases years later - thyroiditis, type 1 diabetes, lupus-like syndromes. One case study followed a 42-year-old man who developed permanent kidney damage after 22 days of undiagnosed DRESS from carbamazepine. He needed lifelong dialysis.
Mortality is around 10%. That’s higher than AGEP (a milder drug rash) and lower than SJS/TEN (a more explosive skin condition). But the real danger is the delay. Patients in the DRESS Syndrome Foundation’s survey waited an average of 18.7 days for diagnosis. During that time, their organs were being destroyed. Every day without stopping the drug and starting steroids increases the risk of death.
How It’s Treated - Steroids, Not Just Stopping the Drug
Stopping the drug is step one. That’s non-negotiable. But stopping it alone isn’t enough. You need to suppress the immune system’s rampage. That’s where corticosteroids come in. Prednisone, usually started at 0.5 to 1 mg per kg of body weight, is the first-line treatment. Studies show 60-70% of patients respond if steroids are started within 72 hours of diagnosis.
But tapering is a minefield. You can’t stop steroids too fast. The immune system can rebound, and organs can flare again. Most patients need 3 to 6 months of tapering - sometimes even longer. Some need second-line drugs like IVIG or mycophenolate, especially if steroids don’t work or cause too many side effects. A new clinical trial at Vanderbilt is testing IVIG plus mycophenolate to reduce steroid dependence. Early results look promising.
For the sickest patients - those with ALT over 1,000, creatinine over 2.0, or breathing trouble - ICU-level care is required. This isn’t a walk-in clinic case. It’s a hospital emergency.

The Future: Screening, Registries, and Prevention
The tide is turning. In March 2023, the FDA approved the first point-of-care test for HLA-B*58:01. It takes 90 minutes. That means before a doctor even writes a prescription for allopurinol, they can check your genetic risk. If you’re positive, they can choose a safer alternative - febuxostat, for example. This isn’t science fiction. It’s happening now.
Taiwan’s success proves prevention works. Universal screening cut DRESS by 80%. The U.S. still lags. But awareness is growing. The DRESS Syndrome Foundation launched a global registry in September 2023 with 47 international sites. Researchers are hunting for biomarkers that predict who will develop long-term autoimmune problems after recovery. That’s the next frontier.
Within five years, experts predict pre-prescription HLA screening will become standard for all high-risk drugs - not just allopurinol and carbamazepine. That could reduce DRESS incidence by 60-70%. The goal isn’t just to treat it. It’s to stop it before it starts.
What Patients Should Do
If you’ve been on any of these drugs - allopurinol, carbamazepine, phenytoin, lamotrigine, vancomycin, sulfonamides - and you develop a rash plus fever after two weeks, don’t wait. Go back to your doctor. Say: "Could this be DRESS?" Ask for a CBC with differential and liver enzymes. If your doctor doesn’t know what you’re talking about, ask for a dermatologist or an immunologist. Don’t let them brush it off as "just a reaction."
Keep a list of every medication you’ve taken in the last 60 days. Bring it to every appointment. If you’re diagnosed with DRESS, get connected with the DRESS Syndrome Foundation. Their patient support network has helped thousands. And if you recover - share your story. You might save someone else’s life.

 Health and Wellness
Health and Wellness
Jaswinder Singh
December 1, 2025 AT 20:46This shit is terrifying. I knew someone who got DRESS from allopurinol and spent three months in the ICU. They lost half their liver function. No one took it seriously until their skin started peeling off like a damn sunburn. Why the hell are we still not screening people before prescribing this stuff? It’s not rocket science.
Bee Floyd
December 3, 2025 AT 16:30Man, I read this whole thing and just sat there in silence. It’s wild how something so quiet can destroy you. I’ve seen doctors shrug off rashes like they’re just a side effect of life. But this? This is a siren song disguised as a pimple. I’m gonna print this out and leave it on my doc’s desk next time I’m in. No more guessing games.
Jeremy Butler
December 4, 2025 AT 04:04The pathophysiological cascade initiated by xenobiotic-induced immune dysregulation, particularly in the context of HLA-associated genetic susceptibility, represents a paradigmatic example of the human organism’s vulnerability to iatrogenic insult. The temporal latency between pharmacological exposure and systemic manifestation underscores the epistemological limitations of contemporary clinical diagnostics, which remain largely reactive rather than prophylactic.
Courtney Co
December 5, 2025 AT 09:59I had a friend who got DRESS from lamotrigine and it changed her life forever-she’s now on lifelong steroids and can’t even hold her baby without shaking. And the worst part? Her doctor told her it was "just stress." I cried for three days. Why don’t they listen? Why do we have to suffer until we’re barely alive before someone says "oh wait, maybe it’s not allergies"? It’s not fair. It’s not right. I’m still mad.
Eric Vlach
December 7, 2025 AT 00:54HLA screening before allopurinol is a no brainer. Why aren’t we doing it everywhere? I mean seriously. We test for everything from blood type to HIV before surgery but we hand out life-threatening meds like candy. I’m not a doctor but even I know this is dumb. If you’re South Asian or have a family history of gout, just ask for the test. It’s 90 minutes. Could save your life. End of story.
Souvik Datta
December 7, 2025 AT 15:29There’s a deeper truth here beyond the medicine. DRESS isn’t just a reaction-it’s a mirror. It shows us how disconnected modern medicine has become from the body’s wisdom. We rush to suppress symptoms instead of listening to what the body is screaming. The fever, the rash, the failing organs-they’re not mistakes. They’re messages. And we’ve trained ourselves to ignore them until it’s too late. We need to heal the system, not just the patient.
Priyam Tomar
December 8, 2025 AT 12:07Everyone’s acting like this is some new discovery but I’ve seen this for years. Allopurinol is a death sentence for anyone over 50 with kidney issues. And don’t get me started on carbamazepine-those things are basically poison for half the population. The real problem? Doctors don’t read. They just prescribe. And patients? They just take it. We’re all just waiting for the next disaster. This isn’t science. It’s Russian roulette with pills.
Jack Arscott
December 9, 2025 AT 05:39So if you’re on allopurinol and you get a rash… just stop it. Like, right now. 🚨 And tell your doctor to check your liver. 🏥 I’m not a doctor but I’ve been there. It’s not worth the risk. Stay safe out there 💪❤️
Irving Steinberg
December 9, 2025 AT 16:16Wow so many people are dying from meds and nobody’s doing anything? I mean come on. We have a whole system built on profit and not care. I’m just here for the memes but also… this is wild. Like why aren’t we banning these drugs already? 🤷♂️