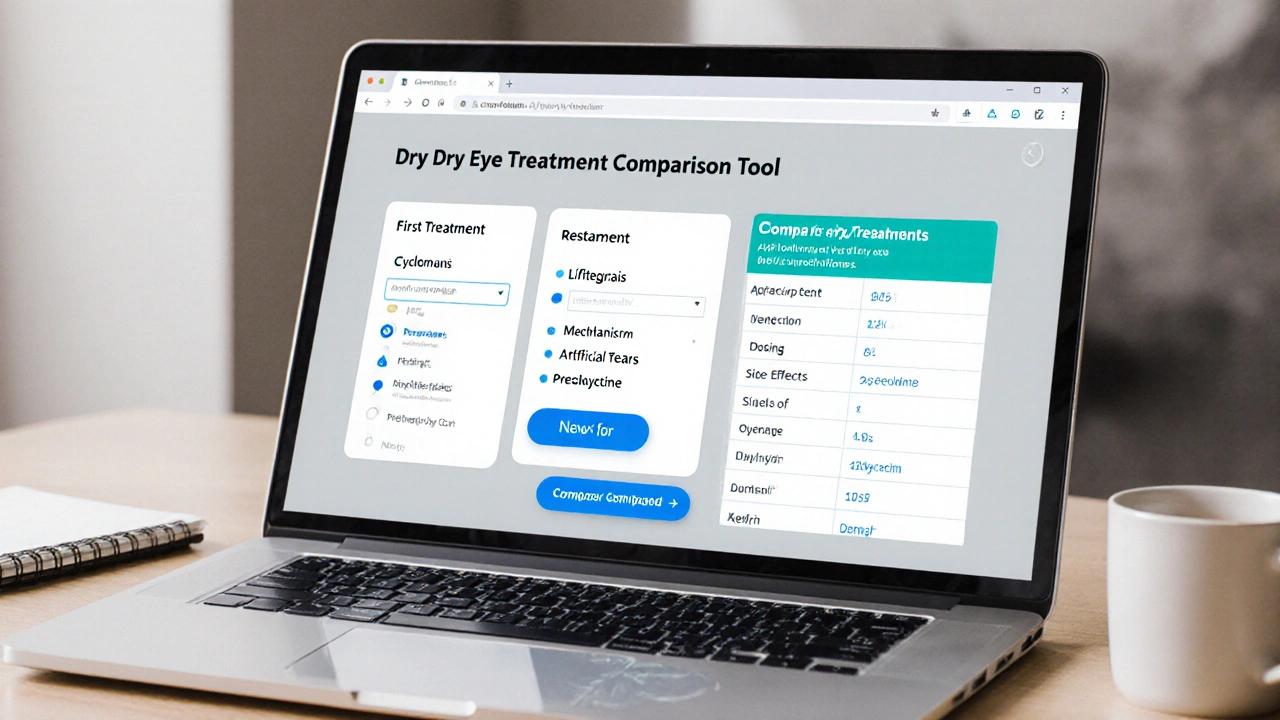
Dry Eye Treatment Comparison Tool
Compare Dry Eye Treatments
Select two treatments to compare key features and find the best option for your needs.
Treatment Comparison Results
Quick Takeaways
- Cyclomune is a prescription cyclosporine eye drop that reduces inflammation in dry‑eye disease.
- Its main rivals are Restasis (another cyclosporine), Lifitegrast (Xiidra), and over‑the‑counter artificial tears.
- Onset of relief: Cyclomune and Restasis can take 4-6 weeks; Lifitegrast often feels faster (2-3 weeks).
- Side‑effects differ: Cyclomune may cause a burning sensation, Lifitegrast can cause dysgeusia, while artificial tears are generally safe.
- Cost varies widely - insurance may cover Cyclomune and Restasis, but Lifitegrast can be pricier without PBS subsidy.
What Is Cyclomune?
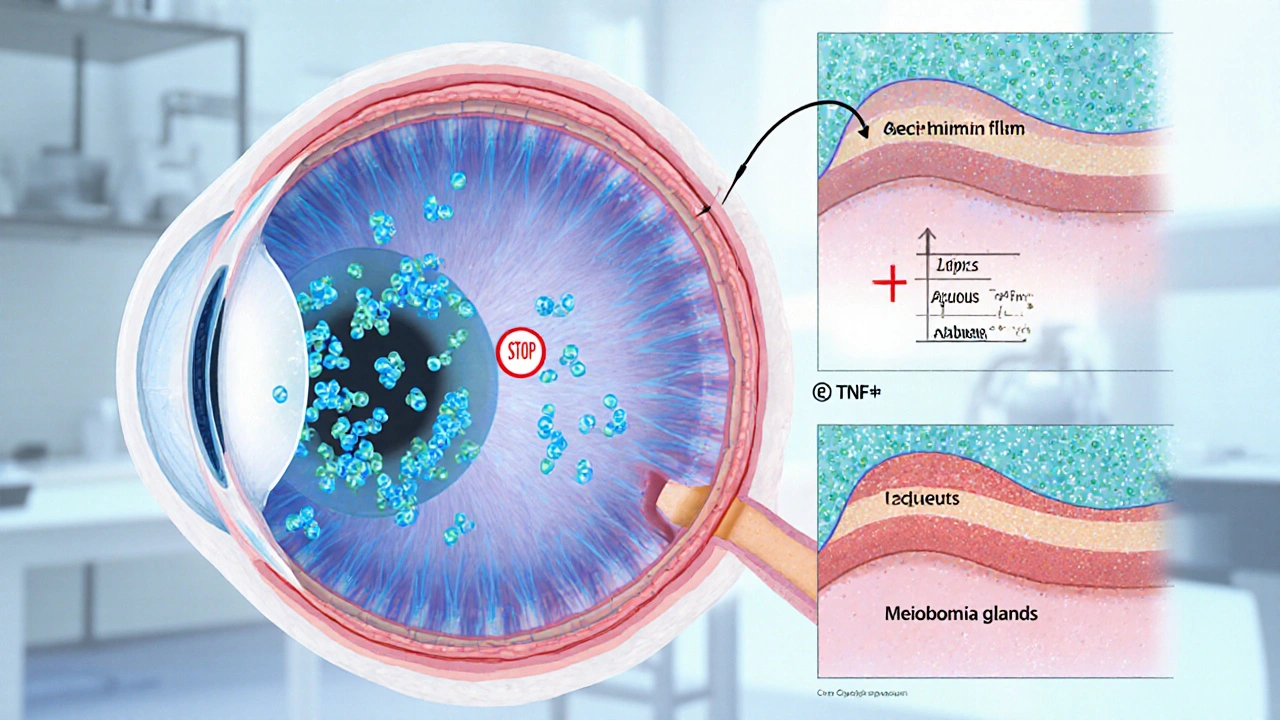
When you hear "dry eye," think of a tear film that’s either not enough or too quick to evaporate. Cyclomune eye drops are a prescription‑only formulation that delivers cyclosporine A directly to the ocular surface. Approved in Australia in 2023, it targets the underlying inflammation that fuels tear‑film instability.
The active ingredient, cyclosporine, is an immunomodulator originally used to prevent organ‑transplant rejection. In the eye, it inhibits T‑cell activation and reduces cytokine release, allowing glands to produce more stable tears over time.
How Does Cyclomune Work?
Cyclosporine binds to cyclophilin inside ocular cells, forming a complex that blocks calcineurin. This stops the transcription of interleukin‑2 and other inflammatory messengers. The result? Less inflammation, better meibomian gland function, and a thicker lipid layer on the tear film.
Because the drug modifies the immune response, it doesn’t provide immediate lubrication. Most users notice a meaningful change after about a month of twice‑daily use.
Top Alternatives to Cyclomune
While Cyclomune is a solid option for many, several other treatments address dry eye from different angles. Below is a quick snapshot of the most common alternatives.
- Restasis - another cyclosporine A formulation, on the market since 2003.
- Lifitegrast (marketed as Xiidra) - a small‑molecule integrin antagonist approved in 2016.
- Artificial tears - over‑the‑counter lubricants ranging from simple saline solutions to preservative‑free gels.
- Ocular steroids (e.g., Prednisolone) - short‑term anti‑inflammatory drops for acute flare‑ups.
- Oral doxycycline - a low‑dose antibiotic that improves meibomian gland health, often used for chronic MGD.
Comparison Table
| Attribute | Cyclomune | Restasis | Lifitegrast (Xiidra) | Artificial Tears | Prednisolone (Steroid) | Doxycycline (Oral) |
|---|---|---|---|---|---|---|
| Active ingredient | Cyclosporine A 0.05% | Cyclosporine A 0.05% | Lifitegrast 5% | Polyethylene glycol / propylene glycol (varies) | Prednisolone acetate 1% | Doxycycline 40mg |
| Mechanism | Calcineurin inhibition → reduced inflammation | Same as Cyclomune | Integrin LFA‑1 antagonist → blocks inflammatory signaling | Lubrication & tear‑film stabilization | Broad anti‑inflammatory, reduces cytokines | Anti‑bacterial, reduces MMP‑9 activity in glands |
| Prescription? | Yes (PBS‑listed) | Yes (PBS‑listed) | Yes (not PBS‑listed) | No (OTC) | Yes, short‑term | Yes, oral |
| Typical dosing | One drop each eye BID | One drop each eye BID | One drop each eye BID | 1‑2 drops as needed | One drop QID for ≤2weeks | One capsule daily |
| Onset of relief | 4‑6weeks | 4‑6weeks | 2‑3weeks | Immediate (minutes) | Immediate to 1week | 4‑8weeks |
| Common side‑effects | Burning, foreign‑body sensation | Burning, blurred vision | Eye irritation, dysgeusia | Transient blur, possible preservative irritation | Increased IOP, cataract risk | GI upset, photosensitivity |
| Cost (AU$ per month) | ≈$45 (PBS subsidy) | ≈$45 (PBS subsidy) | ≈$120 (no subsidy) | ≈$10‑$20 (OTC) | ≈$30 (short course) | ≈$25 |
| Best for | Chronic inflammatory dry eye, MGD‑related | Similar to Cyclomune, long‑term users | Patients needing faster relief, post‑LASIK dry eye | Mild dryness, occasional irritation | Acute flare‑ups, allergic conjunctivitis | Severe Meibomian gland dysfunction |
Decision Criteria - What Matters Most?
Before picking a product, ask yourself these questions:
- Is the dry eye primarily inflammatory? If yes, cyclosporine (Cyclomune, Restasis) or lifitegrast are logical.
- How quickly do you need relief? Artificial tears give instant comfort, but they don’t fix the root cause.
- Do you have insurance coverage? In Australia, both Cyclomune and Restasis are PBS‑listed, dramatically lowering out‑of‑pocket cost.
- Are you comfortable with potential side‑effects? Burning sensation is common with cyclosporine; steroid use demands eye‑pressure monitoring.
- Do you have comorbidities like rosacea or acne? Low‑dose doxycycline can hit two birds with one stone.
Best‑For Scenarios
Cyclomune shines for patients with moderate‑to‑severe dry eye driven by inflammation and for those who qualify for PBS subsidy.
- Best for: Long‑term tear‑film rehab, meibomian gland dysfunction, patients seeking a once‑daily routine after the initial 2‑week loading phase.
- Not ideal for: Immediate relief needs, budget‑tight patients without subsidy, or those intolerant to ocular burning.
Restasis offers a familiar alternative for those who have used cyclosporine before and are comfortable with its side‑effect profile.
Lifitegrast (Xiidra) is the go‑to when you want faster symptom control and can handle a mild after‑taste.
Artificial tears remain essential as adjuncts, regardless of which prescription drop you choose.
How to Start Using Cyclomune Safely
- Get a prescription from your optometrist or ophthalmologist.
- Wash hands thoroughly, then tilt your head back and pull down the lower eyelid.
- Instill one drop in each eye twice a day, preferably morning and evening.
- Avoid touching the tip of the bottle to any surface.
- Wait at least 5minutes before applying any other eye product.
- Schedule a follow‑up after 4-6weeks to assess improvement and any side‑effects.
If you experience persistent burning beyond the first two weeks, discuss with your doctor-sometimes a preservative‑free formulation or a short course of artificial tears can ease the transition.
Common Pitfalls and How to Avoid Them
- Skipping doses. Because the drug works by modulating immunity, missing several days can reset progress.
- Using the wrong storage. Keep the bottle at room temperature; extreme heat can degrade cyclosporine.
- Mixing with other drops without waiting. Give a 5‑minute window to prevent dilution.
- Ignoring eye‑pressure checks. Though rare, cyclosporine can raise intra‑ocular pressure; annual monitoring is prudent.
When to Switch or Combine Therapies
If after 8weeks you haven’t seen a 30% improvement in symptom scores (e.g., OSDI questionnaire), consider one of these options:
- Add Lifitegrast for a dual‑mechanism approach.
- Introduce preservative‑free artificial tears 4-6 times daily.
- Discuss a brief steroid taper (prednisolone) for flare‑ups.
- Evaluate oral doxycycline if meibomian gland plugging persists.
Frequently Asked Questions
How long does a bottle of Cyclomune last?
A 10mL bottle provides roughly 150 drops. At twice‑daily dosing, that works out to about 2½months.
Can I use Cyclomune if I wear contact lenses?
Yes, but remove lenses before applying the drop and wait at least 15minutes before reinserting to avoid dilution.
Is Cyclomune safe for pregnant women?
There’s limited data, so doctors usually recommend postponing cyclosporine therapy until after pregnancy unless benefits clearly outweigh risks.
Will insurance cover Cyclomune?
In Australia, Cyclomune is listed on the PBS, so most patients pay a modest co‑payment. Private insurance often mirrors this coverage.
Can I use Cyclomune with other prescription drops?
Yes, but maintain a 5‑minute gap. For steroid drops, limit use to 2weeks and monitor pressure.

Next Steps for You
1. Book an appointment with your eye‑care professional and discuss whether Cyclomune fits your diagnosis.
2. If you’re cost‑sensitive, ask about PBS eligibility and possible generic alternatives.
3. Start a symptom diary (once daily) to track improvement - this makes follow‑up conversations data‑driven.
4. Keep a small bottle of preservative‑free artificial tears on hand; they’ll smooth over any initial burning.
5. Re‑evaluate after 6weeks. If you’re still struggling, bring the diary to your doctor and explore combination therapy.
Dry eye can feel relentless, but the right mix of medication, lubricants, and lifestyle tweaks often restores comfort. Whether you choose Cyclomune, Restasis, Lifitegrast, or a simpler tear substitute, understanding each option’s strengths makes the decision less guesswork and more confidence.

 Health and Wellness
Health and Wellness
Jennifer Haupt
October 1, 2025 AT 14:33When evaluating Cyclomune against other dry‑eye therapies, it is essential to consider both the pharmacologic mechanism and the systemic implications. The calcineurin inhibition provided by cyclosporine addresses the inflammatory root cause, which differentiates it from mere lubricants. Additionally, PBS subsidy in Australia markedly reduces the financial barrier for many patients. However, the four‑to‑six‑week onset period demands realistic expectations and adherence. Ultimately, this option is well‑suited for chronic inflammatory dry eye where long‑term management outweighs the need for immediate relief.
Loren Kleinman
October 1, 2025 AT 14:41From a philosophical standpoint, the choice between Cyclomune and its alternatives can be seen as a pursuit of balance between symptom relief and underlying disease modification. One might argue that treating the inflammation directly is a more holistic approach, whereas artificial tears are merely a symptomatic band‑aid. The simplicity of the cyclosporine molecule belies its complex immunological impact, a fact often overlooked in casual discussions. Moreover, the cost considerations, especially under a PBS scheme, introduce an ethical dimension concerning accessibility. In the end, the patient must weigh immediate comfort against long‑term ocular health, recognizing that each pathway carries its own set of trade‑offs.
Sabrina Goethals
October 1, 2025 AT 16:46So, looking at the table you can see that Cyclomune and Restasis are basically twins, they share the same active ingredient, same dosing schedule, and even the same side‑effects profile, which is kinda interesting. The main diffrence is the branding and the fact that Cyclomune is newer on the Austraian market, so you might get a little more hype about it, lol. If you’re after something that’s cheap, the PBS subsidy makes both of them a solid choice, but if you need faster relief Lifitegrra might be the way to go, even tho it’s pricier. Also, don’t forget that artificial tears can be used alongside any of these medicaitons, they won’t interfere if you wait the proper 5‑minute gap. In short, pick what matches your timeline, budget, and tolerance for that burning sensation.
Sudha Srinivasan
October 1, 2025 AT 16:55While the science is solid, one must not ignore the moral responsibility of prescribing expensive drugs when cheaper, effective OTC options exist.
Jenny Spurllock
October 1, 2025 AT 18:10Onset speed is a key factor that separates cyclosporine formulations from lifitegrast.
Bart Cheever
October 1, 2025 AT 19:33Cyclomune presents itself as a commendable addition to the armamentarium against dry eye, yet its utility must be examined through a series of practical lenses. First, the pharmacodynamics of cyclosporine A target the inflammatory cascade, a mechanism that is undeniably beneficial for patients whose keratopathy stems from chronic inflammation. Second, the cost structure, tempered by the PBS subsidy, places this medication within reach of a broader demographic, thereby reducing socioeconomic disparity. Third, the dosing regimen-one drop per eye twice daily-offers a level of simplicity that encourages compliance, though the initial burn can be disconcerting for some users. Fourth, the latency period of four to six weeks before noticeable improvement demands patience and diligent follow‑up, which, if neglected, may lead to premature discontinuation and perceived inefficacy. Fifth, the side‑effect profile, though generally mild, includes ocular burning and a transient foreign‑body sensation that might be mistaken for irritation from preservative‑containing artificial tears. Sixth, the comparative analysis with Restasis reveals that the two formulations are virtually identical in composition, raising questions about any clinical advantage beyond branding. Seventh, when pitted against lifitegrast, the latter offers a faster onset of two to three weeks, albeit at a substantially higher out‑of‑pocket cost and without PBS support. Eighth, artificial tears remain indispensable as adjuncts, providing immediate relief while the immunomodulatory medication takes effect. Ninth, the potential for increased intra‑ocular pressure, though rare, underscores the necessity for periodic eye‑pressure monitoring. Tenth, patient education regarding proper storage-room temperature away from direct heat-prevents degradation of the active compound. Eleventh, the necessity of a five‑minute interval before applying any additional ocular product avoids dilution and preserves therapeutic efficacy. Twelfth, clinicians should assess for contraindications such as active ocular infection before initiating therapy. Thirteenth, the integration of a symptom diary can objectively track therapeutic response and guide clinical decisions. Fourteenth, if after eight weeks there is insufficient improvement, a combination therapy approach, such as adding lifitegrast or a short course of steroids, may be warranted. Fifteenth, the overarching goal is to restore tear‑film stability and improve quality of life, which requires a holistic strategy beyond a single pharmacologic agent. In sum, Cyclomune is a valuable tool, but its success hinges on patient selection, adherence, and vigilant monitoring.
Maude Rosièere Laqueille
October 1, 2025 AT 19:41For anyone starting Cyclomune, remember to keep a small bottle of preservative‑free artificial tears handy; they’ll soothe the initial burning and help you stay consistent with the treatment schedule.
Amanda Joseph
October 1, 2025 AT 20:56Oh great, another eye drop that burns like a tiny dragon – just what we needed.
Kevin Aniston
October 1, 2025 AT 21:05Look, I get that the burn can be off‑putting, but think of it as a tiny reminder that the medication is actually doing its job at the cellular level. If you push through the first couple of weeks, you’re likely to see a measurable reduction in discomfort and a more stable tear film. It’s also helpful to pair the drops with a gentle, preservative‑free artificial tear regimen, applying a few minutes after the cyclosporine to keep the ocular surface lubricated. And don’t forget to schedule that follow‑up appointment around the six‑week mark; it gives your eye care professional a chance to assess response and tweak the plan if needed. Consistency is key, and the payoff, while not instant, can be a dramatic improvement in daily comfort.
kiran kumar
October 1, 2025 AT 22:20Honestly, throwing a pricey prescription at a problem that can be managed with cheap drops seems like a marketing ploy rather than genuine care.
Brian Johnson
October 1, 2025 AT 22:28I understand the frustration, and many patients feel the same way. It’s important to weigh the long‑term benefits against short‑term costs, especially when chronic inflammation is at play. If you’re unsure, a trial period with close monitoring can provide clarity without fully committing.
Jessica Haggard
October 1, 2025 AT 23:43Hello friends! If you’re from a multicultural background, you might notice that eye‑drop tolerance varies with diet and lifestyle, so feel free to share your experiences.
Alan Clark
October 1, 2025 AT 23:51It’s awesome to see a community sharing knowledge – keep spreading the word, and let’s help each other find the best eye‑care solutions.
Mark Anderson
October 2, 2025 AT 01:06What a brilliant rundown! The blend of scientific detail and practical advice makes it easy for anyone to decide whether Cyclomune fits their lifestyle and budget.
Shouvik Mukherjee
October 2, 2025 AT 01:15Let’s remember that each patient’s journey is unique, and fostering a supportive environment encourages open dialogue about treatment choices.
Ben Hooper
October 2, 2025 AT 02:30Onset time matters for many users.
Marjory Beatriz Barbosa Honório
October 2, 2025 AT 02:38Even if you’re feeling a bit hesitant about the initial sting, think of it as a stepping stone toward lasting comfort – you’ve got this, and the community’s cheering you on.
G.Pritiranjan Das
October 2, 2025 AT 03:53Stay positive; the right combination will bring relief.
Karen Wolsey
October 2, 2025 AT 05:16Sure, because nothing says ‘effective treatment’ like a pricey drop that makes you feel like you’re sprinkling liquid fire on your eyeballs.
Trinity 13
October 2, 2025 AT 05:25Let’s cut through the sarcasm and focus on the facts: Cyclomune’s mechanism of calcineurin inhibition directly addresses the inflammatory basis of dry eye, which is a substantial advantage over purely lubricating agents. While the burning sensation can be off‑putting, it is a known and temporary side‑effect that typically subsides with continued use. Moreover, the cost advantage provided by PBS subsidies makes it an accessible option for many patients, unlike lifitegrast, which remains expensive and less covered. By integrating preservative‑free artificial tears as an adjunct, users can mitigate the immediate discomfort while waiting for the therapeutic effect to manifest over the recommended four‑to‑six‑week period. Consistency, patient education, and regular follow‑up are the keystones of success with this therapy, ensuring that the potential benefits are fully realized without unnecessary complications.