
When you have diabetes and take medication to control your blood sugar, drinking alcohol isn't just about moderation-it's about survival. A single drink can send your blood glucose plummeting, sometimes hours after you've finished, and you might not even realize it's happening. This isn't a rare edge case. Alcohol and diabetes medications interact in ways that can land you in the emergency room, especially if you're on insulin or sulfonylureas. The risk isn't theoretical. In 2023, nearly 13% of all hypoglycemia-related ER visits among diabetic patients were tied directly to alcohol consumption. That’s over 100,000 avoidable hospital trips in the U.S. alone last year.
How Alcohol Triggers Hypoglycemia
Your liver is the body’s glucose factory. When your blood sugar drops, it breaks down stored glycogen and turns proteins and fats into glucose to keep you stable. Alcohol shuts that factory down. It doesn’t just slow it down-it turns off the lights, locks the door, and throws away the key. The liver prioritizes metabolizing alcohol over everything else. That means no glucose production. For someone on diabetes meds, this is a perfect storm.
Insulin and sulfonylureas like glipizide or glyburide force your body to lower blood sugar. When alcohol blocks your liver’s ability to make more, your blood sugar keeps falling. Studies show alcohol can reduce glucose production by up to 37% for up to eight hours after drinking. That’s why people wake up in the middle of the night with blood sugar at 40 mg/dL-hours after their last drink. The body’s natural warning signs-shaking, sweating, hunger-are often muted by alcohol’s sedative effects. You might feel fine until you pass out.
Which Medications Carry the Highest Risk?
Not all diabetes drugs react the same way with alcohol. Some are far more dangerous than others.
- Insulin: The biggest risk. Alcohol can extend hypoglycemia danger for up to 24 hours. Even if your blood sugar looks normal after dinner, it can crash overnight. A 2023 Mount Sinai study found that 41% of insulin users who drank alcohol had at least one nocturnal low in the following 24 hours.
- Sulfonylureas (glyburide, glimepiride, glipizide): These drugs stimulate your pancreas to release more insulin. When combined with alcohol, they increase hypoglycemia risk by 2.3 times, according to a 2020 meta-analysis. The effect is strongest when taken on an empty stomach.
- Metformin: This one’s tricky. It doesn’t directly cause low blood sugar, but alcohol increases the risk of lactic acidosis-a rare but deadly buildup of acid in the blood. The FDA’s boxed warning says acute alcohol use raises this risk by 5.7 times. Symptoms? Rapid heartbeat, deep muscle pain, nausea, confusion. These can be mistaken for drunkenness.
- Chlorpropamide: An older sulfonylurea, rarely used now, but still prescribed in some cases. It can cause a disulfiram-like reaction: flushing, vomiting, rapid heartbeat-even after one drink. Avoid it completely if you drink.
Big takeaway: If you’re on insulin or sulfonylureas, alcohol is a high-stakes gamble. If you’re on metformin, you’re not off the hook-you just need to watch for different symptoms.
What Counts as a "Safe" Drink?
The idea that "low-carb" alcohol is safe is a myth. A vodka soda with lime sounds harmless, but it’s not the alcohol that’s the problem-it’s the timing, the amount, and what else you’re eating.
Here’s what the American Diabetes Association recommends in 2023:
- Women: No more than one drink per day
- Men: No more than two drinks per day
- One drink = 12 oz beer, 5 oz wine, or 1.5 oz distilled spirits
But here’s the catch: It’s not about the drink-it’s about the context. A mojito has 24 grams of sugar from the syrup and fruit. A glass of sweet dessert wine has 8-14 grams. A vodka soda has 0. That’s why the ADA says: "A mojito on an empty stomach at happy hour is significantly riskier than a glass of wine with dinner."
Choose wisely:
- Best: Dry white wine (under 1g sugar per 5 oz), light beer (under 5g carbs), vodka or gin with soda water and lime
- Avoid: Sweet wines, cocktails with soda, juice, or syrup, hard ciders, liqueurs
And never, ever drink on an empty stomach. Always pair alcohol with food that contains carbohydrates. A sandwich, a small bowl of beans, or even a few crackers can give your liver something to work with instead of letting your blood sugar crash.

Real Stories, Real Consequences
People don’t realize how sneaky this interaction is until it happens to them.
On Reddit, a user named SugarFreeSince19 wrote: "I had three tequila shots at a party. My friends thought I was drunk. I was slurring, dizzy, pale. They left me on the couch. I woke up in the ER with a blood sugar of 42. No one knew I had diabetes."
Another user on the ADA’s community forum described three episodes where they needed glucagon injections after drinking two beers while using an insulin pump. "I checked my glucose before bed-it was 110. I thought I was fine. I woke up at 3 a.m. shaking, drenched in sweat. My CGM showed 38. I had no idea it would hit me hours later."
These aren’t outliers. A 2024 survey of 1,245 people with diabetes found that 73% had experienced at least one alcohol-related low in the past year. Nearly a third needed help from someone else to treat it.
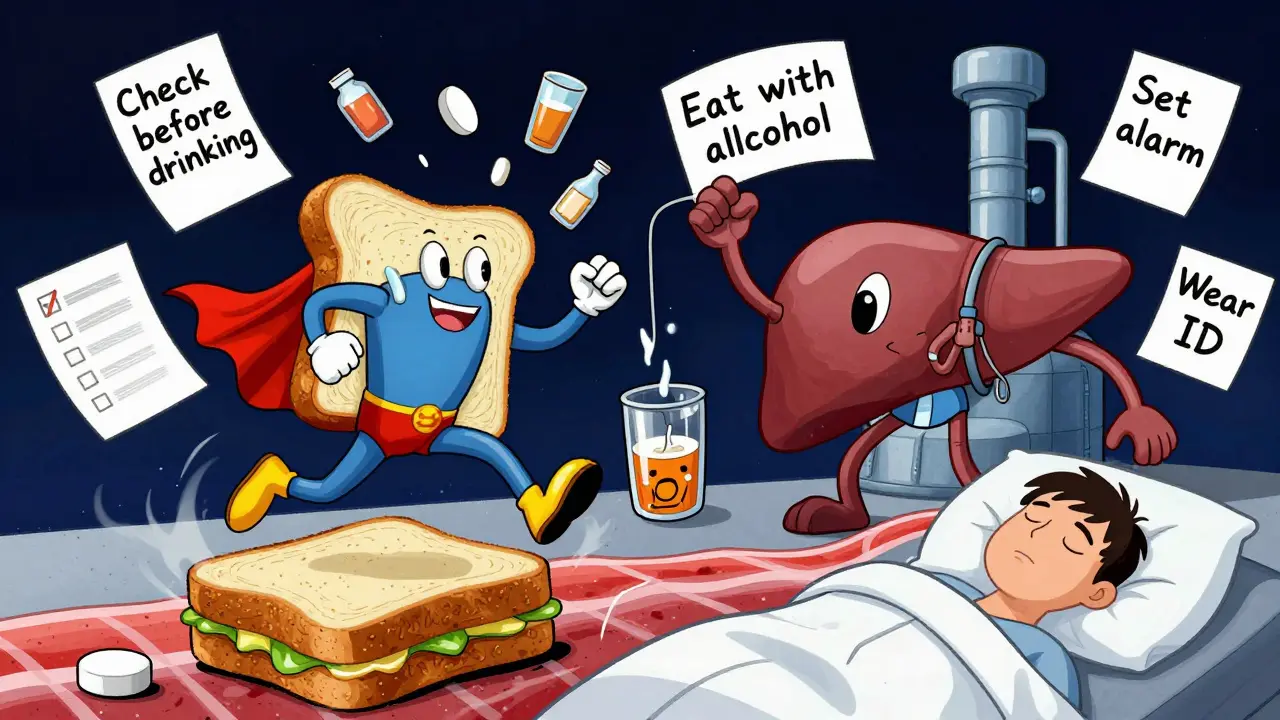
How to Stay Safe: A Practical Checklist
If you choose to drink, follow these steps. Skip any one of them, and you’re increasing your risk.
- Check your blood sugar before you drink. If it’s below 100 mg/dL, eat something with carbs. Don’t drink on an empty stomach.
- Always eat while drinking. Choose complex carbs and protein-whole grain bread, nuts, cheese, beans. Avoid just snacks like chips or pretzels.
- Monitor for 24 hours. Alcohol’s effects can last all night. Set an alarm to check your glucose before bed and again in the morning. Use a continuous glucose monitor (CGM) if you have one. Dexcom’s G7 system now has an alcohol alert feature.
- Wear medical ID. If you pass out, someone needs to know you have diabetes. This reduces emergency response time by nearly half, according to Kaiser Permanente data.
- Tell someone. Make sure at least one person you’re with knows you have diabetes and that alcohol can cause dangerous lows. Teach them how to use glucagon if needed.
- Don’t rely on how you feel. Alcohol masks hypoglycemia symptoms. Dizziness? Confusion? Fatigue? These could be low blood sugar-not intoxication.
What About Non-Alcoholic Beer or Wine?
Non-alcoholic beer and wine still contain trace amounts of alcohol (usually 0.5% or less). For most people, this is safe. But if you’re on insulin or sulfonylureas, even small amounts can contribute to hypoglycemia, especially if consumed in large quantities. It’s better to treat them like regular alcohol-check your numbers, eat with them, and monitor afterward.
Some "zero-alcohol" products are misleading. Always check the label. If it says "alcohol-free," it’s safe. If it says "non-alcoholic," it may still have enough to matter.
Emerging Solutions and Future Trends
The medical community is catching up. In 2024, a pilot study showed that drinking alcohol within four hours after dinner reduced nighttime lows by 31%. Why? Because your liver is still processing food, so it has more fuel to balance out the alcohol’s effects.
CGM companies are now building alcohol alerts into their apps. Dexcom’s G7, released in late 2023, can detect patterns linked to alcohol use and warn users of potential lows hours later. The American Diabetes Association is funding machine learning models to predict individual risk based on medication, liver function, and drinking habits.
But the biggest change? Doctors are asking about alcohol. In 2018, only 54% of primary care providers screened diabetic patients for alcohol use. By 2023, that number jumped to 78%. The AUDIT-C questionnaire-a simple three-question tool-is now standard in many clinics. It’s not about judgment. It’s about safety.
Final Reality Check
You don’t have to quit alcohol to manage diabetes. But you need to treat it like a medication-with clear rules, timing, and monitoring. If you’re on insulin or sulfonylureas, alcohol is a high-risk variable. If you’re on metformin, it’s a warning sign, not a green light. The numbers don’t lie: 12.7% of hypoglycemia ER visits are tied to alcohol. That’s preventable.
Ask yourself: Is a drink worth risking a seizure, a coma, or an ambulance ride? The answer isn’t the same for everyone. But if you’re unsure, the safest choice is to skip it. Your future self will thank you.
Can I drink alcohol if I have type 2 diabetes and take metformin?
Yes, but with extreme caution. Metformin doesn’t cause low blood sugar on its own, but alcohol increases the risk of lactic acidosis-a dangerous buildup of acid in your blood. The FDA warns that drinking even moderately while on metformin raises this risk by 5.7 times. Symptoms include rapid heartbeat, muscle pain, nausea, and confusion. If you drink, do so only with food, limit to one drink per day, and never binge. Avoid alcohol entirely if you have liver disease or kidney problems.
Why does alcohol cause low blood sugar hours after drinking?
Your liver stops making glucose to focus on breaking down alcohol. This process can last 8-24 hours, depending on how much you drank and your liver health. If you’re on insulin or sulfonylureas, your body keeps lowering blood sugar without the liver’s backup. That’s why lows happen at night, after you’ve gone to sleep, or the next morning. It’s not a delayed reaction-it’s a shutdown of your body’s natural glucose production.
Are sugar-free cocktails safe for people with diabetes?
The sugar-free part helps, but it’s not enough. Alcohol itself blocks your liver’s ability to release glucose. Even a vodka soda can cause a dangerous drop if you’re on insulin or sulfonylureas. The lack of sugar doesn’t eliminate the risk-it just removes one layer. Always eat food with alcohol, check your blood sugar before bed, and monitor for 24 hours.
Can I drink alcohol if I use an insulin pump?
Yes, but you need to be extra careful. Insulin pumps deliver steady doses of insulin, which can keep lowering your blood sugar even after you stop drinking. Many users report unexpected lows 6-12 hours later. The ADA recommends reducing your basal rate by 10-20% if you plan to drink, but only under the guidance of your provider. Always check your glucose before bed and set alarms to wake up and check again. Consider using a CGM with alerts.
What should I do if I feel dizzy or confused after drinking?
Don’t assume you’re just drunk. Check your blood sugar immediately. If it’s below 70 mg/dL, treat it with 15 grams of fast-acting carbs (like 4 oz of juice or glucose tablets). Wait 15 minutes and check again. If you can’t check or you’re too confused to treat yourself, get help. Glucagon can be administered by a friend or family member. If you’re alone and can’t get help, call 911. Alcohol masks hypoglycemia symptoms-what feels like intoxication could be a medical emergency.

 Health and Wellness
Health and Wellness
Prateek Nalwaya
February 16, 2026 AT 16:19Man, I never realized how sneaky alcohol can be with diabetes till I saw that stat about 100K ER visits. I’m diabetic, on metformin, and I used to think a vodka soda was ‘safe’-turns out my liver was just taking a nap while my glucose went into freefall. Now I always eat a peanut butter sandwich before drinking, and I set three alarms. One for bedtime. One for 2 a.m. One for when I wake up. I’m not saying I don’t drink-I’m saying I drink like a scientist now.
Philip Blankenship
February 16, 2026 AT 20:07So I’ve been on insulin for 12 years and I still drink-just not like a normal person. I used to think ‘I’m fine’ after two beers, then woke up in the hospital once with a BG of 39. Now I check before, during, after, and again at 3 a.m. I don’t even touch alcohol if I’m stressed or tired. It’s not about willpower-it’s about physics. Your liver can’t multitask, and your meds don’t care if you ‘feel fine.’